Influence of Environmental Stress and Male Infertility-A Clinical Evaluation
Elizabeth Mathew K, Padmalatha C, Ranjitsingh AJA*
Elizabeth Mathew K1, Padmalatha C1, Ranjitsingh AJA2*
1NCARE IVF Centre, MS University, Parappanangadi, Malappuram, Chennai, India
2Department of Biotechnology, Prathyusha Engineering College, Chennai, India
Corresponding Author:
Elizabeth Mathew K
Padmalatha C, Ranjitsingh AJA
Influence of Environmental Stress and Male Infertility-A Clinical Evaluation
Electronic J Biol, 16:5
E-mail: ajargnr@gmail.com
Received Date: October 21, 2020; Accepted Date: November 17, 2020; Published Date: November 24, 2020
Citation: Elizabeth Mathew K, Padmalatha C, Ranjitsingh AJA.Influence of Environmental Stress and Male Infertility-A Clinical Evaluation. Electronic J Biol, 16:S1
Copyright: © 2020 Elizabeth Mathew K. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Infertility is becoming a significant problem globally. To find out the epidemiology of infertility particularly male infertility a study was carried out in a South Indian state. In the present study from the couples visiting a fertility clinic in the Kerala state of India for primary infertility treatment and consultation 750 families were chosen for socio-demographic and clinical study. From the study it was observed that 55.87% of males,41.33% of females,2.13% of both partnersand 0,67percent of unknown factors are responsibleforinfertility. The sociodemographic and clinical study of the identified infertile males showed that all are literate,and 73.98% were in the age group 31-40 years,78.24% were unable to attain fatherhood within 5 years after marriage.Among the 419 males identified with infertility 78.26 percent are working as software professionals usingcomputers, laptops, WI-FI ambience, mobile phones and other microwave radiating devices for over 8 hours per day either in India or abroad having every chance of exposure to electromagnetic radiofrequency radiation(nonionizing radiations) and thermal emission. Clinical evaluation of the infertile males showed that deformities in the semen is the major reason (80.19%) for infertility. However other factors like endocrine dysfunctions (10.26%), and varicoceole in genital part (4.62%) also influence the immunity. In the present survey, four types of sperm disorders were observed. This includeoligoasthenoteratozoospermia (OAT) in 35% of the cases, asthenoteratozoospermia (AT) in 40% of the sample, Teratospermia (T) in 5% of the males and mixed of all these problems in 13 percent of males. The study showed that the incidence of Asthenoteratozoospermia is significantly higher (P<0.05) than the other disorders. Next to AT, OAT prevalence is high. The long hours of exposure tomicrowave radiation emitting digital devicesare believed to induce stress oxidative changes in male reproductive physiology followed by DNAdamagesin the sperm cells thereasons for male infertility. Lifestyle changes likefood habit, dress code, obesity, hormonal changes, work pressure, and certain medications may be the other reasons to strengthen semen defects. Due to COVID-19 lockdown online learning and job work carried out through mobile phones, computer laptops, and WI-FI ambiance and other radiation-emitting gadgets for several hours. So children at and reproductive adults involved in online programme for several hours should plan for their reproductive safety.
https://myseoblog.blogdon.net/
https://myseoblog.blogaaja.fi/
https://myseoblog.jimdosite.com/
https://myseoblog.edublogs.org/
https://myseoblog.websites.co.in/
https://myseoblog47.wordpress.com/
https://myseoblog.waarnnnnnnbenjij.nu/
https://myseoblog.jigsy.com/
https://szeith-rhounds-kliagy.yolasite.com/
https://myseoblog-40.webselfsite.net/
https://myseoblog.mystrikingly.com/
https://myseoblog.splashthat.com/
https://myseoblog.webnode.com.tr/
https://myseoblog.odoo.com/
https://myseoblog.creatorlink.net/
https://whiteseotr1-s-site.thinkific.com/
https://myseoblog.estranky.cz/
https://65390c7d9a166.site123.me/
https://myblogseoooo.blogspot.com/
https://myseoblog.hashnode.dev/
https://whiteseotr1.wixsite.com/myseoblog
https://myseoblogg.weebly.com/
https://sites.google.com/view/myseoblogg/
https://codepen.io/myseoblog/pens/public
https://myseoblogg.livejournal.com/
https://wakelet.com/@myseoblog87204
https://www.homify.com/users/9537482/myseoblog/
https://theomnibuzz.com/author/myseoblog/
https://lessons.drawspace.com/profile/323508/myseoblog/
https://my.desktopnexus.com/myseoblog/
https://writeupcafe.com/profile/myseoblog/
https://www.pearltrees.com/myseoblog
https://www.easyfie.com/myseoblog
https://pharmahub.org/members/27544
https://www.zupyak.com/u/myseoblog/posts
https://www.metroflog.co/myseoblog
https://www.fuzia.com/fz/myseoblog-myseoblog
https://tr.pinterest.com/whiteseotr1/
https://my.getjealous.com/myseoblog
https://micro.blog/myseoblog
https://www.tumblr.com/blog/myseobloggsblog
https://hub.docker.com/u/myseoblog
https://fire.blogfree.net/?act=Profile&MID=1342100
https://myseoblog.pixnet.net/blog
https://myseoblogg.seesaa.net/
https://www.threadless.com/@myseoblog/activity
https://neocities.org/site/myseoblog
https://myseoblog.amebaownd.com/
https://teletype.in/@myseoblog
https://ubl.xml.org/users/myseoblog S6t3Bh9Gwo
https://educatorpages.com/site/myseoblog/
https://myseoblog.onlc.fr/
Keywords
Teratospermia; Asthenote ratozoospermia; MaleInfertility; Oligoasth enoteratoz oospermia; Radiations
Introduction
Infertility is the inability of a sexually active, noncontracepting couple to achieve pregnancy in one year [1].Infertility, by itself, does not threaten physical health but has a substantial impact on the psychological and social well-being of couples. Infertility can result in several emotional stresses. Couples often describe the hope and despair cycle, as they hope each month that they will finally conceive, then despair when once again, it does not happen. Men and women experience the stress and grief in marital life because of infertile marriage. Hence infertility is of public health importance, especially in developing countries, because of its high prevalence and its severe social implications. Global estimates report that 60-80 million couples suffer from infertility every year. In the infertile family that men are responsible for 40% infertility, women also contribute 40% and 20% of both sexes [2].According to an estimate, the infertile Indian population is expected to touch billions by 2035[3]. All India Institute of Medical Sciences (AIIMS) has reported that over 12-18 million couples in India are developing infertility every year. It is stated that while the sperm count of a normal Indian adult male used to be 60 million/ml three decades ago, it now stands at around 20 million/ml. It was observed that male infertility is the primary reason for the inability to conceive, especially between the age group of 29 to 35 due to a combination of low sperm concentration or reduced sperm motility or abnormal morphology[4].Many studies suggest that the quality of semen is declining across the world. A meta-analysis of 61 articles published demonstrates a clear reduction in sperm counts from 113X106 to 66X106 and semen volume from 3.4 to 2.75 ml between 1940 and 1990 [5]. These findings have been confirmed by subsequent studies in the United Kingdom [6,7] France [8], and New Zealand [9]. In Finland also the global trend of impaired male reproductive health prevails [10].The outcome of all these studies conclude that globally a serious problem is blooming about the deteriorationsemen parameters. The deterioration in semen quality is also linked to the increase in testicular cancer, andchanges inlifestyle factors, such as smoking, alcohol, drug use and obesity [5-10]. In addition to life style modifications, occupational exposure plays an important role in semenDNAfragmentation (SDF) and male infertility[11] .Globallyfor 15-70% impotency in couplesmale factoris responsible [12,13]. Though semen analysis is the cornerstone for male infertility assessment, changes in sperm DNAis an important acumen to analyse the reason to predict the reproductive outcome [14],A scientometric analysis of 2121 articles related to sperm DNA fragmentation (SDF) and male infertility shows that SDF starts even at the stage of spermatogenesis. Thesperm DNA integrity in ejaculated sperm is very importantfactor for successful fertilization, embryo development, implantation and pregnancy [15] The lack of thermoregulation of scrotal temperature causes testicular hyperthermia, which leads to genital heat stress . This is detrimental to spermatogenesis and results in spermatozoa of inferior quality. Both the epididymal sperm and testicular germ cells are sensitive to damage by heat stress [16]. Varicoceles also cause SDF and semen quality deterioration. Of the several reasons for varicocoele development,heat stress, continuous sitting postures while operating laptop or mobile,radiationsand subsequent oxidative stress are important reasons [16,17]
Further unhealthy lifestyle, socio-demographic factors lack of physical activity, occupational stress, pollution, poor diet, alcohol consumption, tobacco usage and smoking are the other factors responsible for the increased rate of infertility in men [18-21].
Abnormalities in the reproductive organs such as ductal obstruction, hypo gonadotropic hypo-gonads, bilateral testicular atrophy, and viral orchitis can cause impotency but these are reversible [22]. In humans, for normal testicular function, the temperature in external genitalia requires a temperature of 2–4°C below body temperature, and this has been maintained by physiological mechanisms in male reproductive parts [23]. But continuous external thermal stress interferes with this function, and testicular tissues and epidydimal region experiences oxidative stress affect the functions of the enzyme kinases in cellular metabolism and action leading to genotoxicity, genomic instability and oxidative stress [24-28]. Scrotal hyperthermia and impairment in spermatogenesis in young males is reported [29-34].
As human exposure to radiofrequency (RF) radiation frompersonalelectronic devices,highfrequency dielectric and induction heaters, broadcast antennas, high power pulsed radars, and medical appliances and environmental pollutants Pollutants like pesticides, environmental toxins, spicyfast food from plastics, disturbs reproductive hormones and reproductive functions [36-38].As the present generation is exposed to all these reproductive inhibitoryintrusions from the external and internal environment it is essential to study this problem with immediate attention. To-day In many countries couples visiting the fertility clinics are increasing day by day and Fertility Centre (ART,IVF) and counselingcenter are sprouting in all places. Most of the couples registering for fertility treatment develop stress, hormonal dysfunctions, anxiety, depression, panic disorder, obsessive-compulsive disorder, post-traumatic stress disorder, and phobias[40-44]. India has become one of the major centres of this global fertility industry, with reproductive medical tourism becoming a significant activity. The Assisted Reproductive Technology Regulation Bill is passed by the Government of India in 2020 [39] to regulate and provide ‘safe and ethical’ procedures to over 27 million infertile couples in India.
In the present study, the prevalence of male infertility and the associated reasons are studied using clinical survey and microscopical examination of semen parameters.
Material and Methods
Sample Collection
For the present study couples visiting the NCAREIVF Centre, in South India for infertility treatment and consultation were chosen (Primary infertility-for first child). Among the visitors who opted for clinical evaluation were further short listed.In the short listed infertility ‘suspected’ cases between the period January 2016 to December 2016 a random selection of 750 couple’s clinical reports werescreened with their consent following the ethical formalities without disclosing their identity.
The couples were interviewed to collect their socio-demographic, occupationaland infertility treatment details .From this screened couples , the male partnerssuspected for fatherhoodfailure were further interviewed based on theirclinical reports available and excluding the following problems like hysterectomy, vasectomy, sexual impotence or castration happening as a complication of a traffic or other incident, or a history of prostate cancer or cancer therapy (chemo and radiotherapy).
Among them 419 male partners have given their consent for further interviewing and they were interviewedusing a questionnaire (A modified versionof John Hopkins hospital, USA male infertility evaluation protocol). From this 419 identified infertile malesamples,100 males in the age group 20-45 years with a barren married life for more than an year were subjected to clinical semen analysis .Samples were collected from this selected group at their convenience withina monthafter giving instructions about theirpre -sample donating procedure followed in the IVF Centre.
The samples were collected in the morning by masturbating masturbating and ejaculating into a special container strictly adhering the standard protocol in an air conditioned chamber adjacent to the clinical laboratory, to limit the exposure of the semen to fluctuating temperature and to control the time between collection and analysis. The sample was collected after a minimum of 2 days and a maximum of 7 days of sexual abstinence. When additional samples were required, the number of days of sexual abstinence was constant as possible at each visit. The instructions concerning the collection of the semen sample were given before collection. The man's name, age and personal code number, the period of abstinence, the date and time of collection, the completeness of the sample, any difficulties in producing the sample, and the interval recorded.
Sperm motility study
The semen sample of each donor was analyzed freshly without any storage. Sperm motility within semen was assessed as soon as possible after liquefaction of the sample, preferably within 30 minutes, following ejaculation, to limit the harmful effects of dehydration, pH, or changes in temperature on motility. Motility was assessed at 37°C.TheWet preparation was placed in the cavity counting slide with adepth of 20 μL. Ten microliter drop was placed, and the drop was covered with 22 mm x 22 mm coverslip (area 484 mmThe slides were examined with phase-contrast optics at 400 magnifications.
The slides were systematically scanned to avoid repeatedly viewing the same area by changing fields often. The fields based on the number of motile sperm seen were avoided (field choice was random). Scoring in a given field was at a random instant. Before the spermatozoa to swim into the field or grid to begin scoring was done. The motility of all spermatozoa within a defined area of the field was assessed. This was most easily achieved by using an eyepiece reticule. The portion of the field or grid to be scored from the sperm concentration was selected. Only on the top row of the grid, the sperm concentration was high. Scanning and count were done quickly to prevent possible errors in counting motile spermatozoa. Progressive motile cells, Nonprogressive motile spermatozoa, and finally, immotile spermatozoa were counted. These three categories of sperm movement were scored at one time, and in larger areas of the grid. The number of spermatozoa in each motility category was tallied with the aid of a laboratory counter. About 200 spermatozoa in a total of at least five fields in each replicate were evaluated to achieve an acceptably low sampling error.
Only intact spermatozoa (defined as having a head and a tail) are counted for sperm concentration assessment. Motile pinheads were counted. If no spermatozoa are observed in the replicate wet preparations, azoospermia was suspected. The entire coverslip was scanned field-by-field systematically. Scanning was started from one corner along the x-axis to the opposite side, then in one field along the y-axis.
Sperm vitality study
The vitality of sperms was studied after staining with Nigrosin-eosin. The stain was prepared by dissolving 0.67g of eosin Y (color index 45380) and 0.9 g of sodium chloride (NaCl) in 100 ml of purified water with gentle heating.Then added 10 g of nigrosin (color index 50420) to the 100 ml of eosin Y solution and boiled. After cooling to room temperature, the content was filtered through filter paper (e.g., 90 g/ m2) to remove coarse and gelatinous precipitates and stored in a sealed dark-glass bottle.
The semen sample was mixed well. From this mixture, a 50μl aliquot of semen was taken out and mixed with an equal volume of eosin-nigrosin suspension. For each suspension smear was made on a glass slide and allowed it to dry in air. The slides were examined immediately after drying, or later after mounting with a permanent non- aqueous mounting medium examined each slide with bright field optics at X1000 magnification and oil immersion. The number of stained (dead) or unstained (vital) cells was tallied with the aid of a laboratory counter. Two hundred spermatozoa were evaluated in each replicate to get an acceptably low sampling error. The average and difference of the two percentages of vital cells from the replicate slides were calculated.
Scoring
During scoring live spermatozoa were identified with had whiteheads, and dead spermatozoa with red or dark pink stain. Spermatozoa with a faint pink head were also assessed as alive. If the stain is limited to only a part of the neck region, and the rest of the head area is unstained, this is considered a-leaky neck membrane, not a sign of cell death and total membrane disintegration. These cells were also assessed as alive. These cells were evaluated as viable.
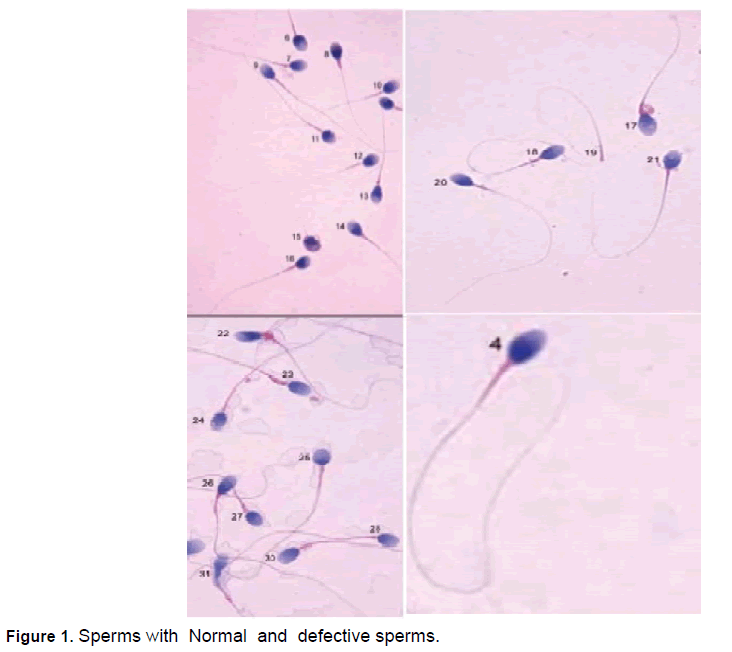
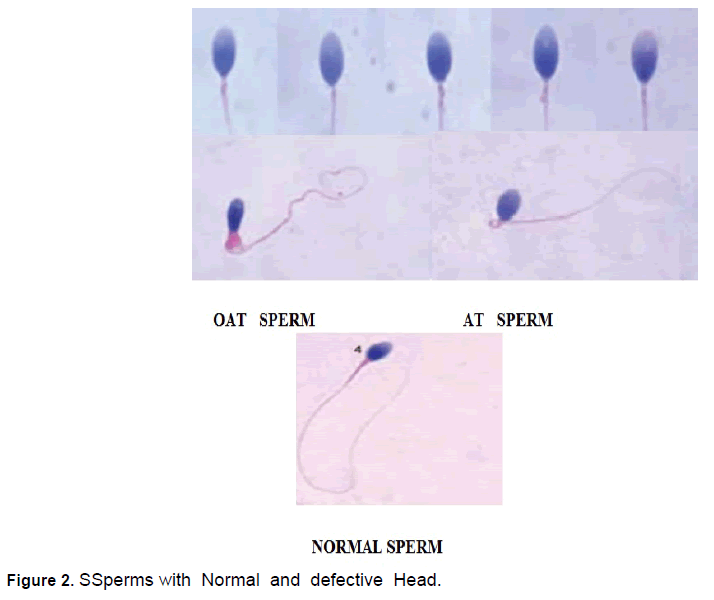
Sperm morphology studies
Staining method
For studying the sperm morphology, Papanicolaou stain was used. The head got stained pale blue in the acrosomal region and dark blue in the postacrosomal part. The midpiece showed some red staining, and the tail was stained blue or reddish. Excess residual cytoplasm, usually located behind the head and around the midpiece, was stained pink or red (Papanicolaou stain) or reddish-orange (Shorr stain) dipping paper. The sperms on five areas on the slide were evaluated under the X100 oil-immersion bright-field objective. The healthy sperm was taken if the sperm head is smooth, regular contoured, and generally oval. They must have a well-defined acrosomal region comprising 40-70% of the head area. Categories of defects were noted. Defects in heads, Neck, and midpiece were recorded.
Results and Discussion
In the present study couples visited the NCAREIVF Centre, in the Kerala state of India between the period January 2016 to December 2016 for infertility treatment andconsultation were chosen (Primary infertility). The couples were interviewed to collect their socio-demographic, occupational and infertility treatment details. From this screened couples, further sub screening was made to identify the couples who were unable to conceive after an year of marriage. They were further interviewed based on their clinical reports available and excluding the following problemslike hysterectomy, vasectomy, sexual impotence or castration happening as a complication of a traffic or other incident, or a history of prostate cancer or cancer therapy (chemo and radiotherapy). Among them a total of 750 couples in the age group 20-45 years suffered with primary infertility. The infertility analysis of the couples revealed that 419 males (55.87%),310 (41.33%) females,16 (2.13%) both genders, and 5 (0.67%),couples with unknown reasons suffer with infertility (Table 1). In the study area males (55.87%) were found more responsible for infertility problems than women (41.33%). As reported earlier (5,7,10) males are more responsible for infertility than females in families. The males identified with the reasons for infertility(419 males) were interviewed for their socio-demographic characteristics and clinical facts (Table 2 and 3).The study revealed that all the infertile males are educatedabove school level and were predominantly in the age group31-35 years (44.39%). Less than 6percent of them suffers with life style aberrations like obesity, BMI, alcoholism, and smoking etc. The socio-demographic fact analysis shows that the males are with good literary rate and this may be the reason for high turn-out for infertility treatment. As the socio-demographic factors are reported [14-17] to be one of the factors responsible for infertility, in the present study also it was found to influence the development of semen disorders and reproductive hormones functional changes.
| Partner responsible for infertility in couples | Number | Percentage |
|---|---|---|
| Males | 4 1 9 | 5 5 .8 7 |
| Females | 3 1 0 | 41 .33 |
| Both Male and Female | 1 6 | 02. 13 |
| Unknown reasons | 0 5 | 00 .67 |
Table 1. Partners responsible for infertility in couples [Percentage] in the study area in India.
| Parameters | Sub details of parameters | Percentage |
|---|---|---|
| 1. Education level | a. Below school education | 0 |
| b. Above school education | 100 | |
| 2.Income level | a. High income group | 36.75 |
| b. Middle income group | 47.74 | |
| c. Low income group | 15.51 | |
| 3.Life style | a. Users of alcohol, tobacco, smoke, other drugs | 3.57 |
| b. Obesity | 3.57 | |
| c. Emotional, doubtful, quarrelsome, aberrant behavior, depressive, negative altitude etc. | 6.32 | |
| 4.Numberof time/month co-habiting with wife | Less than 5 times | 36.76 |
| More than 5 times | 63.24 | |
| 5.Duration interval after marriage | 2-3 years | 31.52 |
| 4-5 years | 42.72 | |
| 6-7 years- | 4.77 | |
| 7-9years | 3.57 | |
| Above 10 years | 17.42 | |
| 6. Age of individual in years | 20-25 | 6.21 |
| 26-30 | 14.56 | |
| 31-35 | 44.39 | |
| 36-40 | 29.59 | |
| 40-45 and above | 5.35 |
Table 2. Showing socio-demographic details of identified infertile males [n=419].
| Clinical Parameters responsible for male infertility(Modified WHO guideline) | Percentage |
|---|---|
| 1.Sexual dysfunction and sexual abnormality(Ejaculation, erective problem) | 5.01 |
| 2.Semen disorders | 80.19 |
| 3. Varicocele | 6.21 |
| 4.Testiculardamage-disease-diabetes, mumps, etc. | 4.53 |
| 5.Endocrine problems | 10.26 |
| 6. congenital disease | 0.48 |
| 7.Laterogenic cause | 3.10 |
| 8.Seminal plasma abnormality | 1.43 |
| 9.Atisperm antibody | 0.72 |
| 10.Un explained infertility | 5.01 |
Table 3. Clinical Parameters responsible for male infertility (Modified WHO guideline) [n=419].
An analysis of clinical parameters showed that semen disorder(80.19%) is the major reason for infertile marriage (Table 3),The other parameters like varicocele (6.21%),sexual dysfunction (5.01%),endocrine disorders (10.29),diseases (4.53%),seminal plasma abnormality (1.43), Laterogenic cause (3.10%), congenital diseases (0.48),antisperm-antibody (0.72%) and unexplainable reasons (5.01),Many workers also confirmed that semen disorders and associated cytological aberrations in sperm cells ,damage to DNA are the major reasons for infertility in males [22,27,29].Further the semen analysis of 100 samples randomly selected from the males with infertility problemsrevealed the factors responsible for semen disorders and what type of defects in spermatozoa interfere with infertility issues. The occupation of the males and semen disorders has a relationship. A critical analysis of the tested males showed that showed that their working environment both in Indiaand abroad with radiation ,thermal stress, exposure to RF-EMF emissions from laptop computers, WI-FI ambience, mobile phones , or other electronic devices interferes with the physiological and biochemical functioning of male reproductive system and genital organs (Table 4, Figure 1 and 2].
| Occupation of the Males | Characteristics of sperm [%] | ||||
|---|---|---|---|---|---|
| N=100 | Normo spermia |
Oligoastheno spermia |
Astheno teratospermia |
Terato spermia |
Mixed defects |
| Employed abroad | 0 | 17.0 | 24.0 | 4.0 | 3.0 |
| Employed In India |
0 | 14.0 | 17.0 | 5.0 | 2.0 |
| Labor type jobs |
0 | 4.0 | 4.0 | 1.0 | 1.0 |
| Fishing | 4.0 | 0 | 0 | 0 | 0 |
| Total | 4.0 | 35.0 | 45.0 | 10.0 | 6.0 |
Table 4. The relationship between different types of sperm Disorders and occupation of the infertile male [N=100].
Among the 100 infertile males tested 48 percent were workingabroadmostly in Middle East countries andreturned to India on holidays, 38 percent are working in Indiain computer and information technology-related jobs and exposed to radiation emitting (RF-EMF) digital gadgets for more than 10 hours per day continuously or intermittently , 10 percent belonged to the labor group, and 4 percent are fishermen, Among the males working abroad, 64%, are doing computer related jobs, 21% in oilrefineries,11% in airports and transport related jobs and the rest,4% are involved in other jobs.
A study on the occupation and prevalence of male infertility among the interviewed persons confirmed a relationship between infertility problems and their occupational environment. It is reported that the climate in Gulf nations are hot many days in a year and these workers are mostly sleeping and living in houses with less protection from environmental radiations.A study in Africa reported [45]that hot weather in Africa is the major reason for male infertility (63.7%). In human body scrotum, pampiniform plexus, and muscles play a role to reduce the body temperature in the genital region 2-4 degree belowthan the other region because thehigher temperatures increases the testicular metabolism without a corresponding increase in blood supply, resulting in local hypoxia, varicocoeles developmentand deleterious effects for the tissue[44-46]. Scrotothermia due to high ambient temperature affects spermatogenesis [47]. In the males studied 10 percent were from local labor groups, involved in bakery, catering ,logistic andfarm related work, and 4 percent are fishermen working in offshore fishing vessels. The incidence of infertility is less in males involved in fishing-related activity. Along with the above mentionedtheir ergonomic condition, co -factors like dietary habits, varicocoeleshormonal changes, less opportunity to co-habit with their spouses, and frequent masturbation were theminor reasons for their reduced sperm production.
Types of sperm disorders
In the present survey, four types of sperm disorders were noticed among the infertile males. They include oligoasthenoteratozoospermia (OAT) in 35% of the cases,Asthenoteratozoospermia (AT) in 45% of the sample, Teratospermia (T) in 10% of the males and mixed of all these problems in 6percent of males. The study shows that the incidence of Asthenoteratozoospermia is significantly higher (P<0.05) than the other disorders (Table 4). Next to AT, OAT prevalence is high.The high occurrence of OATand AT in 80% of the males are associated the functional damages in the scrotal part, epididymis, spermatogenesis, varicocoeles and related hormonal activities oxidative stress disturbing the mitotic division of the stem cells located close to the basement membrane of the seminiferous tubules changes in DNA methylation and histone modification leading to DNA fragmentation were reported as the major reasonsfor sperm disorders [46-51].
The quality of the produced sperms isdamaged by electromagnetic radiation emitted by mobile cellular phones, Wi-Fi networks a [52-54]. In the present study also, it is observed that male workers doing computer-related jobs are more prone to infertility problems than others as reported previously [54-56].
Oxidative stress (OS) also plays an independent role in male infertility, with 30% to 80% of infertile men having elevated seminal reactive oxygen species levels (ROS). ROS can negatively affect fertility via a number of pathways, including interference with capacitation and possible damage to the sperm membrane and DNA, which may impair the sperm's potential to fertilize an egg and develop into a healthy embryo [57]. The oxidative stress and associated molecular changes are responsible for 30%–80% of male infertility [58-60]. The RF radiations emitted from cell phones penetratethrough the exposed tissuesinducesheat andoxidative stress [61],that led to alterations after one spermatic cycle in ejaculated sandepididymal sperms[62-68].
Recently due to COVID-19 lockdown, children are compelled to sit before mobile phone or computers even from the tender age for online study. So children and youth are made to sit for online courses under the thermal and radiation ambience of mobile phones, computer laptops, and WI-FI for long hours. So the reproductive functioning of such digital kids may be impaired in the future.According to US EnvironmentalProtection Agency (EPA)the recommended safe level of radiation unit from a laptop exposure levels is between 0.5 milligauss (mG) and 2.5 mG. but this can be achieved if the following conditions are followed. If the laptop is kept by the user at a distance of 1 inch the user is exposed to a radiation unit of 25 up to 500 mG, and if it is kept at a distance of 1foot user is exposed to a radiation unit of 0.4 up to 20 mG. The ideal distance between the user and the laptop or computer system is 1-3feet and in that distance the user will get a radiation of <0.1 up to 1.5 mG. Federal Communication Commission (FCC) (a scientific legislative body of the US government) has recommended a minimum distance of 20 cm between the laptop and the user.Further there is a protocol for safe mobile and WI-FI use. FCC of the U.S. Government, has given a guidelines that the Specific Absorption Rate (SAR) for Cellular Telephones must be less than 1.6-W/kg averaged over 1 gram of actual tissue (SAR value is a measure of the maximum energy absorbed by a unit of mass of exposed tissue of a person using a mobile phone, over a given time or more simply the power absorbed per unit mass).SAR value of a phone has to be mandatorily declared by the company that has made the phone but is it followed properly is a question. For examplea study shows that the mobile phone XiaomiMi A1 has SAR value of 1.75 W/kg which is found to be emitting the highest amount of radiation. If the SAR value from the mobile phone is high the radiation is high Whether this safety level is followed by children using mobile phone for online courses is to be monitored. The US Department of Health states that children and young people under16 should be encouraged to use mobile phones for essential purposes only” and a medical doctors appeal (signed by more than 1,000 physicians) states “Children below the age of 8 should not use cell phones and cordless phones; children and adolescents between the ages 8 and 16 should also not use cell phones or only use them in the case of an emergency”.
Conclusion
The infertility analysis of the couples revealed that 55.87% of males, 41.33% of females, 2.13% of both genders,and 0.67% couples with unknown reasonsare responsible for infertile marriage. The socio-demographic fact analysis shows that the males are with good literary rate and this may be the reason for their high turn-out for infertility treatment. The socio-demographic factors were found to influence the development of semen disorders and reproductive hormones functional changes.From the present study it is understood that the quality of the male gametes and spermatogenesis, and semen quality are deteriorated by heat, as well as radiations, from digital gadgets like computer laptop, mobile phones that are emitting RF-EMF radiations. In the present studyfour types of sperm disorders, oligoasthenoteratozoospermia (OAT) in 35% of the cases,Asthenoteratozoospermia (AT) in 45% of the sample, Teratospermia (T) in 10% of the males and mixed of all these problems in 6percent of males were noticed. The high occurrence of OAT and AT in 80% of the males are associated the functional damages in the scrotal part, epididymis, spermatogenesis, varicocoeles and related hormonal activities oxidative stress disturbing themitotic division of the stem cells located close to the basement membrane of theseminiferous tubules changes inDNA methylation and histone modificationleading to DNA fragmentation were reported as the major reasons for sperm disorders Suchextrinsic factorsinduce oxidative stress and molecular damages in DNA. So along with semen analysis, molecular study at DNA, RNA and centriole level study must be made in males suffering with infertility before going for remediation process. In the on-going online courses for children and reproductive youths attention must be paid to safe guard them from radiations from communicating electronic devices.
References
- World Health Organization. (2010).WHO laboratory manual for the examination and processing of human semen:Fifth edition.
- Kumar N, Kant AS. (2015).Trends of male factor infertility, an important cause of Infertility: A review of literature.J Hum Reprod Sci. 8(4):191–196.
- Lotti F, Maggi M. (2018). Sexual dysfunction and male infertility. Nat Rev Urol. 15(5):287-307.
- Katerina ATurner, Amarnath R, Samantha S, et al.(2020). Male Infertility is a Women’s Health Issue-Research and Clinical Evaluation of Male Infertility Is Needed . Cells.9:990.
- Carlsen E, Giwercman A, Keiding N, et al. (1992). Evidence for decreasing quality of semen during past 50 years. BMJ. 305(6854):609-613.
- Irvine S, Cawood E, Richardson D, et al. (1996). Evidence of deteriorating semen quality in the United Kingdom: birth cohort study in 577 men in Scotland over 11 years. BMJ. 312(7029):467-471.
- Sripada S, Fonseca S, Lee A, et al. (2007). Trends in Semen Parameters in the Northeast of Scotland. J Andrology. 28:313-319.
- Auger J, Kunstmann JM, Czyglik F, et al. (1995). Decline in semen quality among fertile men in Paris during the past 20 years. N Engl J Med.332:281-285.
- Birdsall MA, Peek J, Valiapan S. (2015). Sperm quality in New Zealand: Is the downward trend continuing? N Z Med J.128(1423):50-56.
- Virtanen HE, Sadov S, Vierula M, et al. (2013) Finland is following the trend-sperm quality in Finnish men. Asian J Androl. 15(2):162-164.
- Agarwal A, Mulgund A, Hamada A, et al. (2015) A unique view on male infertility around the globe. Reprod Biol Endocrinol. 26:13:37.
- Sharlip ID, Jarow JP, Belker AM, et al.(2002). Best practice policies for male infertility. Fertil Steril.77(5):873-882.
- Wang C, Swerdloff RS. (2014).Limitations of semen analysis as a test of male fertility and anticipated needs from newer tests. Fertil Steril. 102(6):1502-1507.
- Baskaran S, Agarwal A, Panner Selvam MK. et al. (2019). Tracking research trends and hotspots in sperm DNA fragmentation testing for the evaluation of male infertility: a scientometric analysis. Reprod Biol Endocrinol.110:2019.
- Durairajanayagam D, Agarwal A, Ong C. (2015).Causes, effects and molecular mechanisms of testicular heat stress. Reprod Biomed Online. 30(1):14-27.
- Agarwal A, Hamada A, Esteves SC. (2012). Insight into oxidative stress in varicocele-associated male infertility: part 1.Nat RevUrol.9:678-690.
- Banks S, King SA, Irvine DS, et al. (2005). Impact of a mild scrotal heat stress on DNA integrity in murine spermatozoa. Reproduction.129:505-514.
- Mittal A, Yadav S, Yadav Singh S, et al. (2015).An epidemiological studyInfertilitylity among urban population of Ambala, Haryana. Int J Interdiscip Multidiscip Stud. 2:124-30.
- Manna N, Pandit D, Bhattacharya R, et al. (2014). A community based studyInfertilitylity and associated socio-demographic factors in West Bengal, India. J Dent Med Sci. 13:13-17.
- Magnusdottir EV, Thorsteinsson T, Thorsteinsdottir S, et al.(2005). Persistent organochlorines, sedentary occupation, obesity and human male subfertility. Hum Reprod. 20(1):208-215.
- Jørgensen N, Joensen UN, Jensen TK, et al. (2012). Human semen quality in the new millennium: a prospective cross-sectional population-based study of 4867 men. BMJ Open. 2(4):e000990.
- 22.. Sijo Parikatil, Ashok A, Sandro C.(2020). Male Infertility: Contemporary Clinical Approaches, Andrology, ART and Antioxidants 2nd ed. Springer Nature Andrology.
- Sultan T. (2018). Al-Otaibi, Male infertility among bakers associated with exposure to high environmental temperature at the work place.J Taibah Univ Med Sci. 13(2):103–107.
- Agarwal A, Desai NR, Ruffoli R, et al. (2008). Lifestyle and testicular dysfunction: a brief update. Biomed Pharmacother. 62(8):550-553.
- Agarwal A, Tvrda E, Sharma R. (2014).Relationship amongst teratozoospermia, seminal oxidative stress and male infertility. Reprod Biol Endocrinol. 12:45.
- Nallella KP, Sharma RK, Aziz N, et al.(2006). Significance of sperm characteristics in the evaluation of male infertility. Fertil Steril. 85(3):629-634.
- Kesari, Kavindra K. (2018). Radiations and male fertility. Reprod Biol Endocrinol.16:1118.
- Silber SJ, Nagy Z, Devroey P, et al. (1997). Distribution of spermatogenesis in the testicles of azoospermic men: the presence or absence of spermatids in the testes of men with germinal failure. Hum Reprod. 12(11):2422-2428.
- Mortazavi SAR, Taeb S, Mortazavi SMJ. (2016). The Fundamental Reasons Why Laptop Computers should not be used your lap. J Biomed Phys Eng. 6(4):279–284.
- Agarwal A, Singh A, Hamada A, et al. (2011). Cell phones and male infertility: a review of recent innovations in technology and consequences. Int Braz J Urol. 37(4):432-454.
- Yefim Sheynkin, Michael J, Peter Y. (2005). David Schulsinger and Eugene Komarof Increase in scrotal temperature in laptop computer users .Hum Reprod.20:452–455.
- Thonneau P, Bujan L, Multigner L, et al. (1998). Occupational heat exposure and male fertility: a review. Hum Reprod. 13(8):2122-2125.
- Mieusset R, Quintana Casares P, Sanchez PLG, et al. (1992). Effects of heating the testes and epididymides of rams by scrotal insulation on fertility and embryonic mortality in ewes inseminated with frozen semen. J Reprod Fertil. 94(2):337-343.
- Ostenson CG. (2002). Lap burn due to laptop computer. Lancet. 23:360(9346):1704.
- Sigman M, Jarow JP. (1997). Endocrine evaluation of infertile men. Urology. 50(5):659-664.
- Hjollund NH, Storgaard L, Ernst E, et al. (2002). Impact of diurnal scrotal temperature on semen quality. Reprod Toxicol. 16(3):215-221.
- Yildirim ME, Kaynar M, Badem H, et al. (2015).What is harmful for male fertility: Cell phone or the wireless internet? Kaohsiung J Med Sci. 31:480-484.
- Toshinobu Miyamoto,Akira Tsujimura,Yasushi, et al.(2012). Male Infertility and Its Causes in Human. AdvUrology. 2012.384520.
- Begum, H, Moniruddin ABM, Nahar K. (2009). Environmental and nutritional aspect in male infertility. J Med.10:16-19.
- Magnusdottir EV, Thorsteinsson T, Thorsteinsdottir S, et al. (2005). Persistent organochlorines, sedentary occupation, obesity and human male subfertility. Hum Reprod.20(1):208-215.
- Kumar D, Salian SR, Kalthur G, et al. (2014). Association between sperm DNA integrity and seminal plasma antioxidant levels in health workers occupationally exposed to ionizing radiation . Environ Res.132:297-304.
- Zhou DD, Hao JL, Guo KM, et al. (2016). Sperm Quality and DNA Damage in Men From Jilin Province, China, Who Are Occupationally Exposed to Ionizing Radiation. Genet Mol Res. 22:15
- Arruda JT. (2009). Occurrence of mutations in loci linked to Y chromosome in the offspring born to individuals exposed to ionizing radiation. Genet Mol Res. 8:938.
- https://www.pmindia.gov.in/en/news_updates/cabinet-approves-the-assisted-reproductive-technology-regulation-bill-2020/
- Wardah A , Fawaz E , Zainab A, et al. (2018). High Proportion of Abnormal Semen Characteristics among Saudi Infertile Couples. Clin Med Diag.8(1):14-22.
- Gunes S, Al- Sadaan M, Agarwal A. (2015). Spermatogenesis, DNA damage and DNA repair mechanisms in male infertility. Reprod Biomed. 31(3):309-319.
- John A, Geoffry N. (2007). De Iuliis Origins and consequences of DNA damage in male germ cells. Rep Bio Medicine. 14:727-733.
- Kumar D, Sujith Raj S, Guruprasad K, et al. (2013). Semen Abnormalities, Sperm DNA Damage and Global Hypermethylation in Health Workers Occupationally Exposed to Ionizing Radiation. PLoS ONE.8(7):e69927.
- Rani DS. (2019).High frequencies of non-allelic homologous recombination (NAHR) events at the AZF loci and male infertility risk in Indian men. Sci Rep.18:6276.
- Gutschi T, Mohamad Al-Ali B, Shamloul R, et al. (2011). Impact of cell phone use on men's semen parameters. Andrologia. 43(5):312-316.
- Rago R, Salacone P, Caponecchia L, et al.(2013). The semen quality of the mobile phone users. J Endocrinol Invest. 36(11):970-974.
- Yildirim ME, Kaynar M, Badem H, et al. (205). What is harmful for male fertility: cell phone or the wireless Internet? Kaohsiung J Med Sci.31(9):480-484.
- Zhang G, Yan H, Chen Q, et al. (2016). Effects of cell phone use on semen parameters: Results from the MARHCS cohort study in Chongqing, China. Environ Int. 91:116-121.
- HeidiDanker-Hopfe, AnaBueno-Lopez, HansDorn GernotSchmid, et al. (2002). Spending the night next to a router-Results from the first human experimental study investigating the impact of Wi-Fi exposure on sleep. Int J Hygiene Env Health.228: 113550.
- Kesari KK, Kumar S, Behari J.(2011). Effects of radiofrequency electromagnetic wave exposure from cellular phones on the reproductive pattern in male Wistar rats. Appl Biochem Biotechnol.164(4):546-559.
- Kesari KK, Agarwal A, Henkel R. (2018). Radiations and male fertility. Reprod Biol Endocrinol 16:118.
- Agarwal A, Singh A, Hamada A, et al. (2011). Cell phones and male infertility: a review of recent innovations in technology and consequences. Int Braz J Urol. 37(4):432-454.
- Agarwal A, Panner Selvam MK, Arafa M, et al. (2019). Multi-center evaluation of oxidation-reduction potential by the MiOXSYS in males with abnormal semen. Asian J Androl. 21(6):565-569.
- Santi D, De Vincentis S, Magnani E, et al. (2017). Impairment of sperm DNA methylation in male infertility: a meta-analytic study. Andrology. 5(4):695-703.
- Panner Selvam MK, Agarwal A. (2018). A systematic review on sperm DNA fragmentation in male factor infertility: Laboratory assessment. Arab J Urol.16(1):65-76.
- Panner Selvam MK, Agarwal A, Pushparaj PN, et al. (2019). Sperm Proteome Analysis and Identification of Fertility-Associated Biomarkers in Unexplained Male Infertility. Genes (Basel).10(7):522.
- Usha Rani M, Srinivasa Baba VSSN, Srivalli G. (2018). Analysis of SAR in Human Blood, Bones and Muscles due to Mobile Waves at 900MHz,1800MHz and 2400MHz. Int J App Eng Res.3:2125-2129.
- Santos H, Camilla Mota M, Letícia Signori C, et al. (2016). Evaluation of Lasting Effects of Heat Stress on Sperm Profile andOxidative Status of Ram Semen and Epididymal Sper Oxidative. Med Cellular Long. 1687657.
- https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/215711/dh_124899.pdf
- German Doctors. (2002). Radio-frequency Radiation Poses a Health Risk. Physicians Demand Overdue Precaution.
- FCC. (2011). Specific Absorption Rate (SAR) For Cell Phones:What It Means For You. 12-22.
- Usikalu MR, Soneye O, Akinpel U. (2019). A radiation from different parts of laptop computers. IJMPERD. 8:153-160.
- IARC. (2013). Non-ionizing radiation, Part 2: Radiofrequency electromagnetic fields. IARC Monogr Eval Carcinog Risks Hum. 102:1-460.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences
