Relationship of ApaI VDR Gene Polymorphism to Type 2 Diabetes Mellitus in Pakistani Population
Madiha Sikander
Department of Biochemistry, University of Lahore, Lahore, Pakistan.
Received date: Septemeber 01, 2017; Accepted date: September 18, 2017; Published date: September 25, 2017
Citation: Sikander M. Relationship of ApaI VDR Gene Polymorphism to Type 2 Diabetes Mellitus in Pakistani Population. Electronic J Biol, 13:4
Abstract
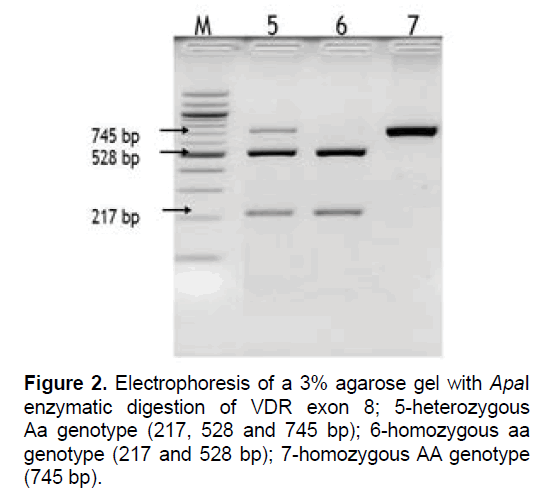
The following study is aimed to describe the relationship of vitamin D receptor (VDR) genetic polymorphism of ApaI to the onset of type 2 diabetes mellitus and obese patients in the local population. One hundred and fifty Type 2 diabetes mellitus (T2DM) subjects and one hundred controls were taken in this study. Genomic deoxyribonucleic acid (DNA) was recovered by standard salt and ethanol precipitation. VDR polymorphism ApaI (rs7975232 G>T) was studied by restriction fragment length polymorphism (RFLP). The presence of all three fragments (217, 528 and 745 bp) after digestion with restriction enzyme indicates heterozygosity (Aa) of ApaI genotype. Results revealed no significant association of ApaI with the T2DM onset and metabolic parameters to support the hypothesis that ApaI may prone macrovascular diabetic complications.
Keywords
Type 2 diabetes mellitus; Polymorphism; RFLP.
1. Introduction
Type 2 diabetes mellitus is a diverse group of metabolic disorders categorized by chronic hyperglycemia as the important global health problem. According to the International Diabetes Federation, diabetes is a type of metabolic disease which affects almost 415 million populations worldwide and will reach to 642 million in 2045. In South Asia, ethnicity is the major risk factor for the T2DM onset. With the limited understanding of the underlying cause of T2DM, a comprehensive acquaintance becomes vital [1,2]. Combination of genetic and environmental factors that contribute to T2DM onset are the life style, dietary habit, body mass index (BMI), hypovitaminosis D and family history. Physical inactivity and obesity are consequences of overweight which contribute to prone T2DM through insulin resistance [3,4].
The incidence of T2DM is related to vitamin D status as it participates in glucose metabolism and insulin release [5,6]. Genetic polymorphism of VDR, vitamin D binding protein (DBP) and cytochrome P450-1alpha genes can affect insulin secretion and cause insulin resistance. A number of VDR variants have been observed in the early 1990s; ApaI, BsmI, EcoRV, TaqI, Tru9I, FokI and CDX2. Recently, one of them contiguous restriction fragment length polymorphism for ApaI has not been found associated with T2DM [7,8].
2. Materials and Method
Blood samples of 150 type 2 diabetic patients attending District Headquarters hospital, Faisalabad, Pakistan were collected on the basis of strict exclusion and inclusion criteria along with 100 normal individuals between January to February 2015. Ethical approval of research protocols was procured from Graduates Studies and Research Board (GSRB), University of Agriculture, Pakistan. The participants were screened for hepatitis B antigen (HBS Ag), hepatitis C (HCV) and human immunodeficiency virus (HIV) prior to scheduled bioassays.
2.1 Exclusion and inclusion criteria
The inclusion criteria for type 2 diabetes mellitus (T2DM) patients was based on world health organization (WHO) (2014) criteria; glycated hemoglobin (HbA1c) (≤ 13.0%), persistence of hyperglycemia (random blood sugar or RBS ≤ 200 mg/dL) and BMI (25-40 kg/m2).
2.2 Physical parameters
The biodata was collected from all case and normal participants. It included age (years), weight (kg), BMI (kg/m2), blood pressure (systolic blood pressure <130 mm Hg and diastolic blood pressure <90 mm Hg were considered non-hypertensive).
2.3 Biochemical parameters
The biochemical parameters were determined by using respective kits (Roche Diagnostics) for plasma glucose levels, HbA1c and vitamin D level following manufacturer’s protocols.
2.4 DNA extraction
Blood samples were collected from patients and healthy donors in 5 ml Ethylenediaminetetraacetic acid (EDTA) coated vacutainer tubes and stored in the refrigerator. Genomic DNA was extracted from the collected blood. Salting out a method for DNA extraction was implied using proteinase K, by peptide hydrolysis and a saturated NaCl solution for cellular dehydration and protein precipitation. Genomic DNA was recovered by standard salt and ethanol precipitation [9].
2.5 Polymerase chain reaction (PCR)
The exon 8 was amplified to study the ApaI polymorphism. The genomic DNA was amplified using specific primers and according to a specific program (PCR thermocycler T100TM, BioRad).
2.6 Enzymatic digestion
After amplification of the VDR fragments with the polymerase chain reaction, all the amplified fragments were digested with the specific enzyme under 25°C temperature for 15 min, allowing to assess the genotype of each individual. One VDR polymorphism was studied: The ApaI (rs7975232 G>T) with its fragments 217, 528, 745 bp.
2.7 Gel electrophoresis
To compare the molecular weight of the DNA fragments, a molecular weight marker (HyperLadder II, Bioline or VC 100 bp Plus DNA Ladder, Vivantis) was used. For agarose gel visualization, UV light using UVITEC system (Uvitec Cambridge) was used.
2.8 Statistical analysis
The results were expressed as mean ± SD (standard deviation) and mean ± SE (standard error). Numerical data were analyzed using paired student's t-test, while one-way analysis of variance (ANOVA) was used to evaluate significant biochemical and molecular results. Allele and genotype frequencies were calculated and the Pearson s’ chi-square (X2) test (the statistical approach used to compare observed data we would expect to obtain according to a specific hypothesis) was used to determine their associations in the case and control participants.
3. Results
3.1 Comparison of biochemical parameters
The comparison of biochemical parameters between type 2 diabetes mellitus and control subjects is mentioned in Table 1.
| Parameter | Diabetic subjects (n=150) | Normal subjects (n=100) | p-Value |
|---|---|---|---|
| FBS (mg/dl) | 145 ÃÆââ¬Å¡Ãâñ 5.54 | 80 ÃÆââ¬Å¡Ãâñ 3.55 | k>0.0001 |
| HbA1c (%) | 7.43 ÃÆââ¬Å¡Ãâñ 0.69 | 4.85 ÃÆââ¬Å¡Ãâñ 0.33 | >0.0001 |
| Vitamin D (mg/dl) | 13.69 ÃÆââ¬Å¡Ãâñ 1.85 | 22.36 ÃÆââ¬Å¡Ãâñ 2.34 | >0.0001 |
Data expressed as mean ÃÆââ¬Å¡Ãâñ SD and p value
SD: Standard Deviation; n: Number of Subjects; FBS: Fasting Blood Sugar; HbA1c: Glycated Hemoglobin.
Table 1. Comparison of biochemical parameters between diabetic and control groups.
3.2 Fasting and postprandial blood glucose levels have been used to diagnose both type 1 and 2 diabetes mellitus globally but fasting blood sugar level is one of the best recommended diagnostic tools (WHO, 2014, 2015). A significantly higher Fasting Blood Sugar (FBS) level and lower vitamin D level were observed in type 2 diabetes mellitus group as compared to control subjects. As present study was conducted to investigate the association of vitamin D to T2DM, inverse significant association of vitamin D with FBS, HbA1c, renal functions profile and lipid profile was noted. However, the extent of the relationship of vitamin D with the onset of T2DM was variable through BMI, along with a weaker relation in people with BMI ≥ 30 kg/m2. Many previous studies have been reported a reduction of relationships of vitamin D with T2DM/dysglycemia hazard after managing for adiposity [10,11]. Vitamin D showed a significant effect on glycemic control via lowering FBS and HbA1c in type 2 diabetes mellitus. Fasting blood glucose was found significantly reduced with respect to high levels of vitamin D by placebo treatment. Thus previous studies revealed that deficiency of vitamin D may be one of the risk factors to develop type 2 diabetes mellitus [12-16].
The prevalence of vitamin D deficiency in present diabetic group was same as in the last survey conducted on Caribbean T2DM patients which found that 42.6% T2DM patients were vitamin D deficient [17].
Association of VDR gene polymorphisms with T2DM
A number of studies have focused on the relationship between T2DM onset and candidate genes. It has been found that deficiency of vitamin D linked with VDR polymorphisms is predisposed to T2DM [18,19]. Receptors for vitamin D are located in the antigen presenting cells, T cells and beta cells of the pancreas. VDR gene has been studied in various populations to find the relationship with susceptibility to T2DM and its complications but outcomes produced conflicting results [18-24]. In this study, ApaI VDR polymorphism was assessed. The aim of this study was to investigate how VDR genotypes and alleles distribution affects the prevalence of type 2 diabetes mellitus in the Pakistani population. Two different main groups were considered in the following study: T2DM patients and control.
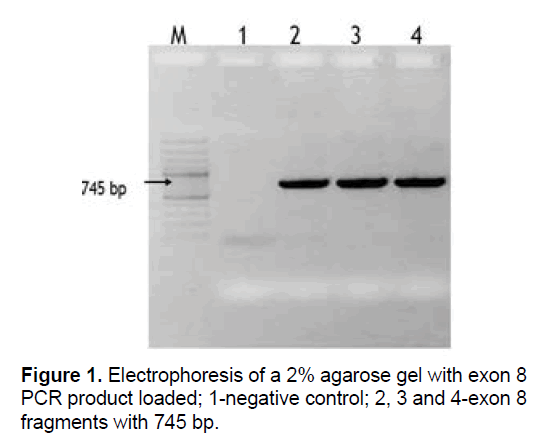
VDR gene (exon 8) was amplified by using PCR to evaluate the ApaI polymorphism in T2DM and control groups. The product of PCR obtained was loaded on agarose gel. The fragment of exon 8 of the VDR gene is given in Figure 1. To verify all distinctive genotypes of exon 8 enzymatic digestion was done (Figure 2). The presence of all three fragments (217, 528 and 745 bp) after digestion with restriction enzyme indicates heterozygosity (Aa) of ApaI genotype.
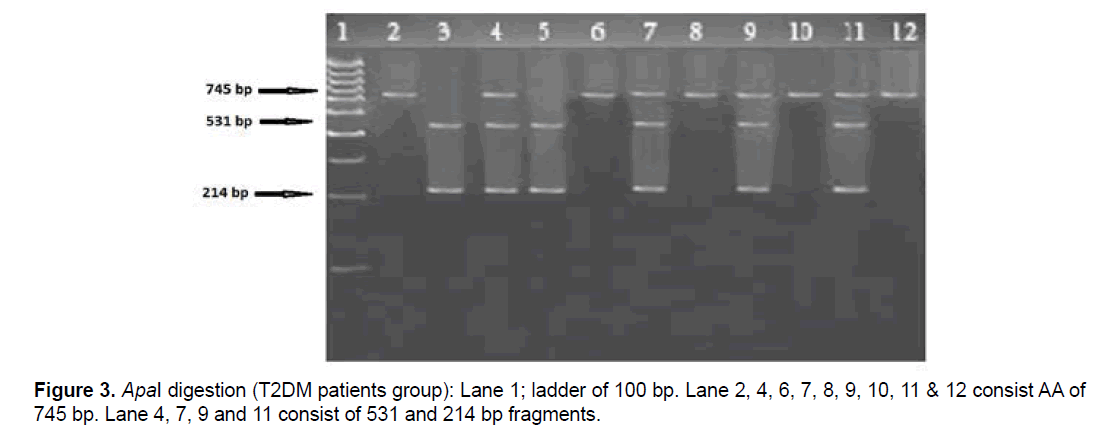
Malecki et al. [25] found no significant association of ApaI with the T2DM onset and metabolic parameters to support the hypothesis that ApaI may prone macrovascular diabetic complications. According to the present study, no statistically significant differences of ApaI allele distributions observed between T2DM subjects and control groups (Table 2). However the overall distribution of ApaI genotypes between healthy control and T2DM groups are aa 3.2%, Aa 46.0%, AA 50.8%. Many acquired and genetic factors may associate with T2DM and its complications but the exact reason of those factors that induce T2DM and its various complications including nephropathy are still not clear [26,27]. Polymorphisms in ApaI genotype of VDR gene among T2DM patients is shown in Figure 3. No significant association observed between VDR gene polymorphism (ApaI) and diabetic complications onset in terms of demographic and biochemical parameters as described by [25,27].
| Genotype | Groups | Total | |||
|---|---|---|---|---|---|
| Control | Patient | ||||
| aa | 4 | 4 | 8 | ||
| 4.0% | 2.6% | 3.2% | |||
| Aa | 54 | 61 | 115 | ||
| 54.0% | 40.7% | 46.0% | |||
| AA | 42 | 85 | 127 | ||
| 42.0% | 56.7% | 50.8% | |||
| Total | 100 | 150 | 250 | ||
| 100.0% | 100.0% | 100.0% | |||
Data expressed as χ2=5.1915.08NS, p=0.075
NS: Non-Significant.
Table 2. Distribution of genotype, allele frequencies and carriage rate of ApaI among patients and controls.
4. Discussion
Type 2 diabetes mellitus is a multifaceted disorder that may be developed due to the interface between environmental or acquired and genetic factors. A number of genes, such as CRP, Calpain 10, eNOS and VDR genes have been involved to develop T2DM [28]. However, VDR gene has more associations to the development of T2DM as compared to all other studied genes.
The present study validated VDR gene polymorphisms were linked with the susceptibility of T2DM in Pakistani population that can be elucidated by the differences of VDR gene variants T2DM and healthy control subjects (p<0.005). No existence of an association between T2DM and VDR polymorphisms linked metabolic parameters, including fasting glucose, HbA1c, liver function tests, renal function tests and lipid profile levels, has been described by observational studies [29,30]. VDR polymorphisms of ApaI genotype were not associated with T2DM in Moroccan population. Distribution of ApaI genotype showed non-significant statistical difference between the healthy subjects and T2DM patient. In agree with present results, the meta-analysis of the association between onset of T2DM and ApaI showed the nonsignificant results [31]. In contrast, a chines study found that ApaI genotype of VDR gene polymorphism was linked with T2DM [32]. Previous studies of candidate gene polymorphism and genome wide association studies have concentrated on the relationship between onset of T2DM and VDR gene, but outcomes have often been fickle among different populations. Mostly the discrepancies between these studies may be because of false positive finding, duplication study lacks power, heterogeneity among studies and heterogeneity transversely studies [33,34].
5. Conclusion
Results revealed no significant association of ApaI with the T2DM onset and metabolic parameters to support the hypothesis that ApaI may prone macrovascular diabetic complications.
References
- Garduno-Diaz SD, Khokhar S. (2012). Prevalence, risk factors and complications associated with type 2 diabetes in migrant South Asians. Diabetes Metab Res Rev. 28: 6-24.
- Bakker L, Sleddering MA, Schoones JW, et al. (2013). Pathogenesis of type 2 diabetes in South Asians. Eur J Endocrinol. 5: 11-13.
- Waugh N, Cummins E, Royle P, et al. (2010). Newer agents for blood glucose control in type 2 diabetes: Systematic review and economic evaluation. Health Technol Asses. 36: 1-248.
- Herder C, Roden M. (2011). Genetics of type 2 diabetes: pathophysiologic and clinical relevance. Eur J Clin Invest. 41: 679-692.
- Ozfirat Z, Chowdhury TA. (2010). Vitamin D deficiency and type 2 diabetes. Postgrad Med J. 86: 18-25.
- Talaei A, Mohamadi M, Adgi Z. (2013). The effect of vitamin D on insulin resistance in patients with type 2 diabetes. Diabetol Metab Syndr. 5: 8.
- Harne AJ, Hagberg J. (2005). Influence of vitamin D receptor gene polymorphisms on changes in insulin sensitivity with aerobic exercise training. JUM. 1: 123-125.
- Lim S, Min Joo K, Sung Hee C, et al. (2013). Association of vitamin D deficiency with incidence of type 2 diabetes in high-risk Asian subjects. Am J Clin Nutr. 3: 524-530.
- Miller SA, Dykes DD, Polesky HF. (1988). A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic Acids Res. 16: 3.
- Alhumaidi M, Adnan AGHA, Mohamed D. (2013). Vitamin D deficiency in patients with type-2 diabetes mellitus in southern region of Saudi Arabia. Maedica (Buchar). 8: 231-236.
- Gandhe MB, Keerthi J, Swapnali MG. 2013. Evaluation of 25(OH) vitamin D3 with reference to magnesium status and insulin resistance in T2DM. J Clin Diagn Res. 7: 2438-2441.
- Middleton J. (2003). The effect of case management on glycemic control in patients with type 2 diabetes. Case Manager.14: 43-47.
- Ronald M. (2004). Lipid and lipoproteins in type 2 diabetes. Diabetes Care. 27: 1496-1504.
- Tushuizen M, Diamant M, Heine R. (2005). Postprandial dysmetabolism and cardiovascular disease in type 2 diabetes. J Postgrad Med. 81: 1-6.
- Bevan JL. (2006). Diabetes mellitus: a review of select ADA standards for 2006. J Nurse Pract. 2: 674-679.
- Hsin O, La Greca AM, Valenzuela J, et al. (2010). Adherence and glycemic control among Hispanic youth with type 1 diabetes: Role of family involvement and acculturation. J Pediatr Psychol. 35: 156-166.
- V̮̩̉̉layoudom-C̮̩̉̉phise FL, Larifla L, Donnet JP, et al. (2011). Vitamin D deficiency, vitamin D receptor gene polymorphisms and cardiovascular risk factors in Caribbean patients with type 2 diabetes. Diabetes Metab. 37: 540-545.
- Omdahl JL, Morris HA, May BK. (2002). Hydroxylase enzymes of the vitamin D pathway: expression, function and regulation. Ann Rev Nutr. 22: 139-166.
- Anderson PH, May BK, Morris HA. (2003). Vitamin D metabolism: New concepts and clinical implications. Clin Biochem Rev. 24: 13-26.
- Florez JC. (2008). Newly identified loci highlight beta cell dysfunction as a key cause of type 2 diabetes: where are the insulin resistance genes? Diabetologia. 51: 1100-1110.
- Ahn J, Yu K, Stolzenberg-Solomon R, et al. (2010). Genome-wide association study of circulating vitamin D levels. Hum Mol Genet. 19: 2739-2745.
- Billings LK, Florez JC. (2010). The genetics of type 2 diabetes: What have we learned from GWAS? Ann Acad Sci. 12: 59-77.
- Wang TJ, Zhang F, Richards JB, et al. (2010). Common genetic determinants of vitamin D insufficiency: a genome-wide association study. Lancet. 376: 180-188.
- Wheeler E, Barroso I. (2011). Genome-wide association studies and type 2 diabetes. Brief Funct. Genomics. 10: 52-60.
- Malecki MT, Frey J, Moczulski D, et al. (2003). VDR gene polymorphisms and association with type 2 diabetes mellitus in a polish population. Exp Clin Endocrinol Diabetes. 111: 505-509.
- Nathanson D, Nystrom T. (2009). Hypoglycemic pharmacological treatment of type 2 diabetes: Targeting the endothelium. Mol Cell Endocrinol. 297: 122-126.
- Arababadi MK, Nosratabadi R, Hassanshahi G, et al. (2010). Nephropatic complication of type-2 diabetes is following pattern of autoimmune diseases? Diabetes Res Clin Prac. 87: 33-35.
- Puri S, Marwaha RK, Agarwal N, et al. (2008). Vitamin D status of apparently healthy school girls from two different socioeconomic strata in Delhi: Relation to nutrition and lifestyle. Br J Nutr. 99: 876-882.
- Nosratabadi R, Arababadi MK, Salehabad VA, et al. (2010). Polymorphisms within exon 9 but not intron 8 of the vitamin D receptor are associated with the nephropathic complication of type-2 diabetes. Int J Immunogenet. 37: 493-497.
- Bid HK, Konwar R, Aggarwal CG, et al. (2009). Vitamin D receptor (FokI, BsmI and TaqI) gene polymorphisms and type 2 diabetes mellitus: a North Indian study. Indian J Med Sci. 63: 187-194.
- Lei LB, Wu JY, Liu A, et al. (2013). Vitamin D receptor gene polymorphisms and type 2 diabetes: A meta-analysis. Arch Med Res. 44: 235-241.
- Xu G, Qiang M, Daijun Z, et al. (2011). Vitamin D receptor gene and aggrecan gene polymorphisms and the risk of intervertebral disc degeneration - A meta-analysis. PLoS ONE. 7: e50243.
- American Diabetes Association. (2012). Standards of medical care in diabetes. Diabetes Care. 35: S11-63.
- Gastaldelli A. (2011). Role of beta-cell dysfunction, ectopic fat accumulation and insulin resistance in the pathogenesis of type 2 diabetes mellitus. Diabetes Res Clin Pract. 1: 60-65.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences