Malaria Prevention and Control Methods Practice and Associated Factors among Rural Households: A Community Based Cross-Sectional Mixed Study
Tsigie Baye Aragie1*, Haileab Fekadu wolde2, Bethelihem Tigabu3, Kindie Fentahun Muchie4
Tsigie Baye Aragie1*, Haileab Fekadu wolde2, Bethelihem Tigabu3, Kindie Fentahun Muchie4
1Ethiopian Field Epidemiology and Laboratory Training Programme, West Belessa Health Office
2Department of Epidemiology and Biostatistics, University of Gondar, Gondar, Ethiopia
3Department of Pediatrics and Child Health Nursing, School of Nursing, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
4Department of Epidemiology and Biostatistics, School of Public Health, College of Medicine and Health Sciences, Bahir Dar University, Bahir dar, Ethiopia
- Corresponding Author:
- Tsigie Baye Aragie
Ethiopian Field Epidemiology and Laboratory
Training Programme
West Belessa Health Office
Tel: 251975132229
E-mail: deacontsige@gmail.com
Received date: October 13, 2021; Accepted date: November 18, 2021; Published date: November 25, 2021
Citation: RAragie TB (2021). Malaria Prevention and Control Methods Practice and Associated Factors among Rural Households: A Community Based Cross-Sectional Mixed Study. Electronic J Biol, S9:01
Abstract
Introduction: Communities’ malaria prevention and control methods practices contribute immensely to sustainable control of malaria. This evidence is quite limited in the study area. Hence, this study aimed to assess Malaria prevention and control methods practice and associated factors among rural households. Method: Community-based cross-sectional mixed quantitative and qualitative study was conducted from April to June 2020, in the West Belessa district. We considered a 740 sample size. We used structured and semi-structured questionnaires for quantitative and qualitative components respectively. We collected the data by interviewing for quantitative and focus group discussion for qualitative. The data was coded and entered using Epi info7 and analyzed using SPSS software. We fitted the binary logistic regression model to identify the associated factors. Result: A total of 738 subjects were included with a 99.7% response rate. Half, 50.9% of respondents had a good malaria prevention and control methods practice. Long-lasting insecticide nets (LLINs) and insecticide residual spray (IRS) were practiced by 21.1% and 80.5% respectively. Poorest, poor, medium and rich wealth quintiles with [AOR=0.45, 95% CI: 0.27, 0.76], [AOR=0.51, 95% CI:0.30, 0.88], [AOR=0.24, 95% CI: 0.14, 0.42] and [AOR=0.21, 95% CI: 0.12, 0.36] respectively Gond ebrareg Kebele [AOR=3.88, 95% CI: 2.43,6.20], female [AOR=0.65, 95% CI: 0.47, 0.90], illiterate [AOR=0.34, 95% CI 0.16, 0.72], poor knowledge [AOR=0.52, 95% CI: 0.36, 0.75] were significantly associated with good malaria prevention practice. All of the FGD participants. Conclusion: IRS and environmental management malaria prevention and control methods practices were relatively high. However, LLINs and other malaria prevention methods were poorly practiced. Wealth index, respondents living kebele, female sex, educational status, and respondents’ malaria prevention knowledge are positively associated with the practice of malaria prevention.
Keywords
Malaria, Practice, Prevention methods, Associated factors
Abbreviations
AOR: Adjusted Odds Ratio; CI: Confidence Interval; FGD: Focus Group Discussions; EFMOH: Ethiopian Federal Ministry of Health; IQR: Inter Quartile Range; IRS: Indoor Residual Spray; MIS: Malaria Indicator Survey; LLINs: Long Lasting Insecticidal Nets; OR: Odds Ratio; SD: Standard Deviation; UNICEF: United Nations Children’s Fund; WHO: World Health Organization; DDT: Dichlorodiphenyl- trichloroethane.
Introduction
Malaria is a protozoan disease transmitted by the bite of infected Anopheles mosquitoes [1]. Globally, there were an estimated 229 million new malaria cases and about 409,000 malaria-related deaths in 2019 [2]. Malaria is one of the leading causes of morbidity and mortality in Africa. The World Health Organization (WHO) African region bearing the highest burden of malaria cases, and death (94%) each [2].
In Ethiopia, the burden of malaria continues to cause a substantial number of morbidity and mortality which accounts for most outpatient visits, and it has been one of the main causes of hospitalization and deaths in the country [3,4]. Approximately 60 percent of the Ethiopian population lives in malarious areas, and 68 percent of the country’s landmass is favourable for malaria transmission [5]. Malaria prevention practices of communities contribute immensely to the sustainable control of endemic diseases such as malaria. Strategic malaria control involves primary prevention which focuses on vector control specifically through the consistent use of insecticidetreated nets and willingness to make the indoor residual spray [6].
Ethiopia had planned to eliminate malaria in the country by 2030 [7]. To achieve this goal the first option is vector monitoring and controlling through Entomological monitoring [7]. The first target of the Ethiopian Ministry of Health is 100% household coverage of at least one LLINs per two family members in the household in all malarious areas [8]. Similarly, EFMOH aims to provide 100% IRS coverage as a key malaria prevention measure in areas where the malaria burden is high [7]. According to the new EFMOH malaria risk stratification, 14.8% of the country’s total population is targeted for IRS [8]. Other vector control activities including larval control through environmental management and chemical larvicides are also practiced in areas where such interventions are appropriate and expected to have a significant impact [8]. However, in 2014 only overall, 32% of households in the malarious area have reached universal LLINs coverage, and 64% of households had at least one LLINs [8].
Evidence from different studies has shown that malaria prevention and control methods practice were affected by different factors such as employment status, marital status, religion, level of education, gender, age, wealth index, the structure of respondents’ houses, and LLINs received by the household [9–12].
Evidence about malaria prevention and control methods practices among households in rural malarious areas of the West Belessa district is quite limited. Hence, the present study aimed to assess malaria prevention and control methods practice and associated factors among rural households in the West Belessa district. This study would help to evaluate the current malaria control programs in the study setup. If properly utilized, this information will urge the decision-makers to strengthen malaria prevention and control interventions effectively and efficiently.
Methods
Study Design and Setting
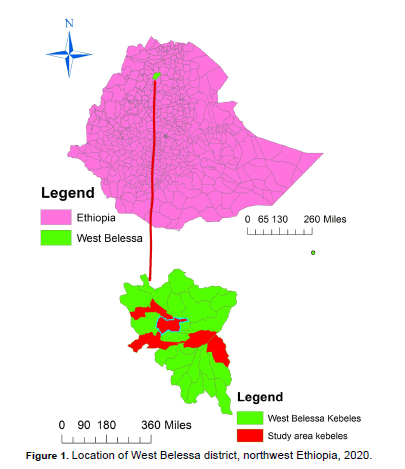
We conducted a community-based cross-sectional mixed quantitative and qualitative study from April to June 2020. This study was conducted in the West Belessa district. It is found in northwest Ethiopia. Ethiopia is one of the countries in East Africa. It has 1.104 million km² areas and 114,963,588 million population in 2020. It has 670 rural districts. West Belessa is one of these districts. West Belessa is, situated at an altitude of 1501 to 3000 meters above sea level. Arbaya town is the capital city of West Belessa district which is located at a latitude and longitude of 12o 15'N and 37° 45'E respectively. From June to August high rainfall is registered with a shortage and heavy rain intermittently and the mean monthly temperature is 33.50c. The district has three climatic zones, hot zone 60%, cold zones 35%, and moderate zones 5%. The district almost all (92.9%) are malarious land area. the estimated total population of the district was 181,974 in 2020. (Figure 1)
Study Population and Sampling Technique
The source population for this study was all households in 24 rural kebeles. There are a total of 24 rural kebeles and one urban kebele in the district. The study population was all households in five selected rural kebeles. The sample size for the survey was determined using a single population formula. We used a 67.7% good practice from a study done in Areka, Ethiopia [13], a 95% CI, and a margin of error of 0.05 to calculate a 336 sample size. By adding a 10% non-response rate and a design effect of two, the final sample size became 740. Five rural kebeles were selected by using the lottery method. The sample size was proportionally allocated based on Keble’s population. We select households using health posts’ household registration by systematic sampling every 13 households. The interviewees were household heads.
Inclusion and Exclusion Criteria
All households’ heads in the selected kebeles who lived there for at least 6 months before the interview were considered for inclusion. Very sick individuals who were unable to communicate were excluded from the study.
Data Collection Methods and Quality Control
The data collection tool was adapted from 2004 WHO/ UNICEF guidelines for core population coverage survey [14] with some modifications. (Data collection tool.pdf) Originally prepared in English then translated into the local language Amharic. Fifteen enumerators who had graduated from university were recruited and trained about the purpose of the study; how to approach respondents; how to obtain written consent and an overview of malaria prevention methods for one day. An interviewer-administered questionnaire was used to collect the quantitative data. The completeness of the questionnaire was checked every day and incomplete questionnaires were returned to the data collectors on the following day for correction by re-visiting the households by the following day. Absent households were revisited on the following days. We conducted Pretesting in one of the malarious kebeles out of the study area.
We conducted a total of four FGDs in four kebeles (Abay tera, Diquana, Ayseg, and Gond ebrareg kebeles). Participants full of information about malaria prevention and control methods were selected for the discussion in each kebeles. The FGD had 7 to 11 participants in each group and comprised a total of 37 study participants in four groups. Each FGD has conducted both recording sounds and taking notes. The content of semi-structured questionnaires was issued about malaria prevention and control methods practice.
Variables of the Study
Malaria prevention and control practice was a dependent variable of the study. A study participant who scored above or equal to the median score of Malaria prevention and control practice questions was considered as having good practice and others considered as having poor practice [13]. The median was seven out of 11 malaria prevention practice questions. Independent variables considered were age; sex, marital status, occupation, religion, ethnicity, address, family size, educational status, and wealth index.
The wealth index was determined by using durable household assets. A total of 18 different durable assets were identified and assigned as dummy variables. The principal component analysis was used to compute the quantile and then re-categorized into five groups (Poorest, Poor, Medium, Rich, and Richest).
Data Processing and Analysis
We used Epi info version 7 to enter and coded quantitative data and exported it to SPSS version 20. We used frequencies and percentages to describe the characteristics of the participants. Binary logistic regression analysis was used to determine the associated factors of malaria prevention and control practice at the level of significance of 0.05 with a 95 % Confidence Interval (CI).
We transcribed qualitative data in the original language of the interview first word by word from the audiotapes and field notes, then translated to English for analysis. The primary theme was produced through manual coding using a pen of different colors, then it was pooled into broader concepts to form main themes.
Ethical Consideration
Approval to carry out the study was sought and obtained from the Ethical Review Board of the authors’ institute. Written consent was obtained from all study participants after a detailed explanation of the purpose of the study.
Results
Socio-Demographic Characteristics
A total of 738 households have participated in this study with a response rate of 99.7%. Above half of the participants, 410 (55.6%) were male (Table 1). The mean age of the respondents was 40.2 (SD= ± 12.24) years. Almost all of the respondents 733 (99.3%) were Orthodox Christian, and the majority of the respondents, 664 (90.0%) were married. Concerning the educational status majority, 648 (87.8%) of the participants were illiterate. Above half of the respondents, 438 (59.4%) had 4-6 family members in their house. The mean household member was 5.01 (SD ± 1.72). The economic status of the respondents was assessed using the wealth index which showed, 19.0%, 20.3%, 19.2%, 18.8%, and 22.6% of the respondents ranked as richest, rich, medium, poor, and poorest respectively. (Table 1)
| Variable | N=738 | Frequency | Percent |
|---|---|---|---|
| Age | 18-24 | 49 | 6.6 |
| 25-34 | 193 | 26.2 | |
| 35-44 | 234 | 31.7 | |
| 45-54 | 165 | 22.4 | |
| 55-64 | 66 | 8.9 | |
| >64 | 31 | 4.2 | |
| Sex | Male | 410 | 55.6 |
| Female | 328 | 44.4 | |
| Religion | Orthodox | 733 | 99.3 |
| Others | 5 | 0.7 | |
| Educational status | Illiterate | 648 | 87.8 |
| Literate | 48 | 6.5 | |
| Formal education | 42 | 5.7 | |
| Marital status | Married | 664 | 90.0 |
| Divorced | 26 | 3.5 | |
| Not married | 35 | 4.7 | |
| Widowed | 13 | 1.8 | |
| Number of family members | <4 | 157 | 21.3 |
| 4-6 | 435 | 58.9 | |
| >6 | 146 | 19.8 | |
| Wealth index | Poorest | 167 | 22.6 |
| Poor | 139 | 18.8 | |
| Medium | 142 | 19.2 | |
| Rich | 150 | 20.3 | |
| Richest | 140 | 19.0 |
Table 1. Sociodemographic characteristics of respondents for Malaria prevention and control methods practice in West Belessa, northwest Ethiopia, 2020.
Respondents Malaria Prevention and Control Methods Practices
Above three-quarters of the households, 582 (78.9%) did not have LLINs (Table 2). A total of 212 LLINs were identified in 156 (21.1%) households; of which 100 (64.1%) received one LLINs and the remaining 56 (35.9%) households received two LLINs from the government. Regarding utilization out of the mosquito LLINs owners, two-third (68.6 %) of them used the LLINs in the previous night of data collection. Of the total LLINs owners 22 (14.1%) of them used LLINs for other purposes.
| Malaria prevention and control methods practice | N=738 | Percent |
|---|---|---|
| At least one LLIN | 156 | 21.1 |
| Use of LLIN in the previous night | 107 | 14.5 |
| IRS | 594 | 80.5 |
| Proofing in windows and doors | 156 | 21.1 |
| Closing windows and doors early at night | 28 | 3.8 |
| Environmental management (compact and drainage) | 568 | 77.0 |
| Clear the vegetation | 297 | 40.2 |
| Participated in Epidemic control | 408 | 55.3 |
| Re-plastering the wall in 6 months of IRS spray | 131 | 17.8 |
| Other prevention methods* | 38 | 5.0 |
*burning of leaves in the house to repel the mosquito, and using Aerosol spray to repel the mosquito
Table 2. Malaria prevention and control methods practice in West Belessa, northwest, Ethiopia, 2020.
In this survey the most frequently used malaria prevention method was IRS (80.5%) of which 608 (82.4%) were didn’t re-plasterer within six months after spray operation has been carried out. The least frequently used malaria prevention methods were closing windows and doors early in the evening (3.8%). About three-fourth (77.0%), of the respondents, participated in environmental measures such as compact and drainage to control malaria and 40.2% of the respondents participated in clearing the vegetation. Above half 408 (55.3%) of the respondents have been participated in epidemic control.
Overall total respondents about half 379 (50.9%), respondents had good practices (with 95% CI, 47.2 - 54.5) and the remaining half 362 (49.1%), of the respondents, had poor malaria prevention and control methods practice. The median practices score for all respondents was four out of a possible 10 points score (IQR=2-4). (Table 2)
In the FGD discussion, the IRS operation has a long history in their locality about half of the respondents explained that their houses was sprayed in the last 12 months. The majority of the discussants participated in the IRS by preparing their house and fetching water for spray preparation. A 50 years old female participant in Abaytera kebele explained "we prepare the house for spray by renewing the wall, take out of materials which we use in the house, we keep away home animals and children for some hours, and fetch the water for spray."
As the discussant expressed there were few refusals and plastering of the wall in six months of spray due to different reasons such as miss-understanding of IRS chemicals; miss-conception of the chemical as a multiplier of other insect nuisance; it kills the honey bees, and the current IRS chemical is less efficacious and expires in a short time to kill mosquitoes than the previous brands (i.e. DDT). A 60 years old male in Gond ebrareg kebele FGD explained "The current yellow color IRS chemical is less efficacious and expires in a short time."
In the discussions, the majority of the participants did not own LLINs. All groups in the discussions indicated that LLINs’ inaccessibility to buy and lack of provision by the local government appeared to contribute to the low household insecticide bed net ownership. A 39 years old male in Abaytera kebele FGD explained "for the last time the LLIN was distributed three years ago." Somewhat surprisingly, in the discussion, some of them mentioned that there was the use of LLINs for others beyond the intended purpose. In Diquana kebele’s FGD participants, "We use the bed net for other purposes due to old age of the LLINs and lack of awareness." Some of the discussants also mentioned that nowadays there is a decrement in the efficacy of LLINs brands.
The discussants participated in environmental management (compact, drain, and clearing the vegetation) in Abaytera FGD "we participate in malaria prevention in environmental management using 1 to 5 group male and female groups and the group leaders organize every activity."
Associated Factors of Malaria Prevention and Control methods Practice (Table 3)
| Variable | Response | Level of Practice | ||||
|---|---|---|---|---|---|---|
| Good (%) | Poor (%) | COR(95%CI) | AOR(95%CI) | P-value | ||
| Resident’s Kebele | Dikuana | 39(5.3) | 70(9.5) | 0.68(0.42-1.11) | 0.62(0.37-1.05) | 0.08 |
| Abaytera | 56(7.6) | 94(12.7) | 0.73(0.47-1.14) | 0.68(0.43-1.09) | 0.11 | |
| Gond ebrareg | 160(21.7) | 48(6.5) | 4.10(2.66-6.32) | 3.88(2.43-6.20) | <0.001 | |
| Tala | 38(5.1) | 48(6.5) | 0.97(0.58-1.63) | 0.99(0.57-1.72) | 0.96 | |
| Ayseg | 83(11.2) | 102(13.8) | 1 | 1 | ||
| Sex | Female | 139(18.8) | 189(25.6) | 0.54(0.4-0.72) | 0.65(0.47-0.90) | 0.01 |
| Male | 237(32.1) | 173(23.3) | 1 | 1 | ||
| Educational status | Illiterate | 317(43.0) | 331(44.9) | 0.38(0.19-0.76) | 0.34(0.16-0.72) | 0.005 |
| Literate | 29(3.9) | 19(2.6) | 0.27(0.61-1.486) | 0.39(0.15-1.04) | 0.06 | |
| Formal education | 30(4.1) | 12(1.6) | 1 | 1 | ||
| Wealth index | Poorest | 82(11.1) | 85(11.5) | 0.37(0.23-0.60) | 0.45(0.27-0.76) | 0.003 |
| Poor | 77(10.4) | 62(8.4) | 0.48(0.29-0.79) | 0.51(0.30-0.88) | 0.02 | |
| Medium | 86(11.7) | 56(7.6) | 0.25(0.15-0.41) | 0.24(0.14-0.42) | <0.001 | |
| Rich | 90(12.2) | 60(8.1) | 0.26(0.16-0.42) | 0.21(0.12-0.36) | <0.001 | |
| Richest | 101(13.7) | 39(5.3) | 1 | 1 | ||
| Knowledge | Poor | 61(8.3) | 117(15.8) | 0.41(0.29-0.58) | 0.52(0.36-0.75 | 0.001 |
| Good | 315(42.7) | 245(33.2) | 1 | 1 | ||
Table 3. Factors associated with malaria prevention and control methods practice in West Belessa District, northwest Ethiopia, 2020.
From the multivariable model, it was found that those individuals who live in Gond ebrareg kebele had about 4 times increased odds of having a good practice as compared with respondents who live in Ayseg kebele [AOR=3.88, 95% CI: 2.43, 6.20] (Table 3). The odds of having good practice were decreased by 35% among female respondents as compared to male respondents [AOR=0.65, 95% CI: 0.47, 0.90]. The odds of having a good practice were decreased by 66% among illiterate respondents as compared to respondents who had formal education [AOR=0.34, 95% CI: 0.16, 0.72]. Moreover, the odds of having a good practice were decreased by 55% among respondents in the poorest wealth quintile as compared to the richest [AOR=0.45, 95% CI: 0.27, 0.76]. Similarly, the odds of having good practice was decreased by 49%, 76%, and 79% among respondents in poor, Medium and rich wealth quintiles respectively as compared with richest wealth quintiles with [AOR=0.51, 95% CI: 0.30, 0.88]; [AOR=0.24; 95% CI: 0.14, 0.42]; and [AOR=0.21 95%CI: 0.12, 0.36] respectively. The odds of having good practice were decreased by 48% among respondents who have poor knowledge about malaria prevention as compared to their counterparts [AOR=0.52, 95% CI: 0.36, 0.75].
Discussion
This study mainly investigated malaria prevention and control methods practices and associated factors among rural households in malarious areas of rural West Belessa.
The major malaria targets of the Ministry of Health are 100% household coverage of LLINs in the household in all malarious areas with the free distribution of LLINs [8]. Since 2005, significantly increased the coverage of the LLINs intervention [15,16]. Despite this, in west Belessa only 21.3% of the respondents owned at least one LLINs in their house. This is much lower as compared with studies done in Woreta and Arba Minch as well as the 2015 MIS (64%) [8,17,18]. The difference is due to lack of access to buy the bed net and lack of affordability as confirmed in the FGD discussion. This evidence is supported by a study done in southern Tanzania [19]. Regarding utilization of the total respondents who owned at least one LLINs 68.6 % of them used it in the previous night of data collection. This is in line with a study done in Gurage and a study done in the Dabat district Amhara region [10,20].
The EFMOH’s National Malaria Strategic plan aims to provide 100% IRS coverage as a key malaria prevention measure in areas where the malaria burden is high. According to this survey, 80.5% of the houses were sprayed with IRS in the past 12 months this is higher compared with the MIS 2015 which was 29%, and a study done in Gondar town [8,21]. But it is lower compared with a study done in Jabi Tehnan, Ethiopia (87.5%) [22]. The difference may be due to the difference in the study area. Because only 14.85 of the country’s total population is targeted for IRS spray [23]. So that, areas targeted for IRS have high coverage of IRS.
In this study, 84.3% of the respondents participated in environmental management (i.e. compact, drainage, and clear vegetation) to control malaria. This is similar to a study done in the Gurage zone and a study done in Eritrea [10,16]. In this study, the respondents report that there were low prevention practices of other malaria prevention methods. i.e. aerosol sprays and burning of leaves which was used by about only 5% of the respondents in total. Similarly, only 3.7% of the respondents used closing windows or doors early to prevent malaria. This is lower comparing with the studies in Pawe and Shewa robit [24,25]. This is due to low knowledge of these prevention methods as confirmed in the FGD which was mentioned by none of the participants. This evidence is also supported by a study done in West Belessa as well as in Nyando Kenya [11,26].
Overall, 50.9% of the study participants had good practice in comprehensive concerning the practice of malaria prevention and control. This is in line with the study done in Amhara National Regional State, Ethiopia, in which 47.1% of the total study participants have good practice towards malaria prevention and control activities [26]. However, it is lower than a study done in Areka (67.7%) [13]. This could be due to study area differences our study has been conducted in rural areas which are difficult to get malaria prevention options such as LLINs and others while other studies were conducted in urban setups.
In this survey, the odds of having a good practice is 35% less among female participants as compared with male participants. This is consistent with a study done in Nigeria (12). This could be due to that male individuals are responsible for malaria prevention activities especially males are responsible to handle prevention activities outside the house in rural households. The odds of having a good practice is 66% less among illiterate respondents as compared with formally educated educational status. As information is the first step for practice households lead by illiterate individuals were less likely to practice malaria prevention practice than formally educated individuals; results from some other researches also reported a higher probability of malaria prevention measures undertaken by educated individuals [27,28].
The odds of having good practice were 55%, 49%, 76%, and 79% less among poorest, poor, Medium, and rich wealth quintiles respectively as compared with the richest wealth quintiles. Households with the lowest economic status were less likely to practice prevention measures than the higher economic status households. Similar to this finding, higher practice amongst households with a higher wealth index has been reported previously in Gurage [10]. This could be because individuals from high wealth index households have better information on access and capacity to buy sample-monetary aerosol sprays, build a favorable house for living and hence are more likely to use bed nets, spray houses and drain compounds. The odds of having good practice are 3 times increased among respondents who live in Gond ebrareg kebele as compared with Ayseg kebele this was related to good malaria prevention knowledge, as evidenced by a study done in West Belessa [29].
As a limitation, this study is unable to establish causality due to the cross-sectional nature of the design. Readers are suggested to consider this into account.
Conclusion
In rural west Belessa; there were good IRS and environmental management malaria prevention practices. However, LLINs and other malaria prevention methods such as using an aerosol spray, screening windows and doors as well as closing windows and doors early were poorly practiced. There was a lack of accessibility and provision of LLINs in the study area. As confirmed through FGD nowadays there is a decrement in the efficacy of IRS and LLINs as compared with the previous brands. Wealth index, malaria prevention knowledge, respondents living kebele, educational level, and respondents' sex were predictors for malaria prevention and control methods practice.
The use of easily accessible personal protection methods such as screening windows and doors; closing windows and doors early at night as well as using aerosol spray and burning of leaves are recommended malaria prevention methods. Programmers, partners, and implementers are recommended to increase the accessibility of LLINs in different options such as free provision and easily accessible at the market. Further research is needed for the efficacy of the IRS and LLIN. Low socioeconomic groups, low educational status, and female individuals need attention in malaria prevention and control programs.
Acknowledgment
First all, we would like to thank the Almighty God for giving us health and strength to perform this project. We would like to thank West Belessa District administrative bodies and community cooperation and permission to conduct the study. We are also thankful for the University of Gondar for their support to conduct the study as well as the data collectors who participated in the study for their commitment.
Funding
President's Malaria Initiative (PMI) mini grant
Competing Interests
There is no competing interest.
References
- World Health Organization (2015). Global technical strategy for malaria 2016-2030. World Health Organization.
- World Health Organization. World malaria report 2020: 20 years of global progress and challenges. In World malaria report 2020: 20 years of global progress and challenges 2020.
- Ethiopian federal ministry of health, National Strategic plan for malaria prevention, control and elimination in Ethiopia, 2010 – 2015, (2002/2003 –2007/2008 EC Addis Ababa, 2009 Mar;
- Aregawi M, Lynch M, Bekele W, et al. (2014). Time series analysis of trends in malaria cases and deaths at hospitals and the effect of antimalarial interventions, 2001–2011, Ethiopia. PLoS One. 9:e106359.
- US-president’s malaria initiative Ethiopia, Malaria-operational-plan. 2017.
- WHO (2007). Regional Office for Africa “Implementation of Indoor Residual Spraying of Insecticides for Malaria Control.” 2007.
- US-president’s malaria initiative Ethiopia (2018). Malaria operational-plan.
- Ethiopian Public Health Institute. Malaria-Indicator-Survey. Vol. 6. 2015.
- Dako-Gyeke M, Kofie HM (2015). Factors influencing prevention and control of malaria among pregnant women resident in urban slums, Southern Ghana. Afr J Reprod Health. 19:44-53.
- Girum T, Hailemikael G, Wondimu A (2017). Factors affecting prevention and control of malaria among endemic areas of Gurage zone: an implication for malaria elimination in South Ethiopia, 2017. Tropical diseases, travel medicine and vaccines. 3:1-9.
- Mbijiwe KK.Factors Influencing Use of Malaria Control Methods among the Residents of Nyando Sub-County, Kisumu County(Doctoral dissertation, JKUAT-COHES).
- Amusan VO, Umar YA, Vantsawa PA (2017). Knowledge, attitudes and practices on malaria prevention and control among private security guards within Kaduna Metropolis, Kaduna State-Nigeria. Sci J Public Health.5:240-5.
- Kebede DL, Hibstu DT, Birhanu BE (2017). Knowledge, Attitude and Practice towards Malaria and Associated Factors in Areka Town, Southern Ethiopia: Community-Based Cross Sectional Study. J Trop Dis.5(3):1-1
- World Health Organization (2004). Guidelines for core population coverage indicators for Roll Back Malaria: to be obtained from household surveys.
- Ethiopian ministry of health FDE. National malaria strategic plan 2014–2020. Addis Ababa Minist Health. 2014.
- Habtai H, Ghebremeskel T, Mihreteab S, et al. (2009). Knowledge, attitudes and practices (KAP) about malaria among people visiting referral hospitals of Eritrea in 2008. J Natl Med Assoc. 4:42-6.
- Alelign A, Petros B (2018). Knowledge, attitudes and practices of malaria transmission and preventive measures in Woreta town, Northwest Ethiopia. BMC research notes. 11:1-5
- Astatkie A (2010). Knowledge and practice of malaria prevention methods among residents of Arba Minch Town and Arba Minch Zuria District, Southern Ethiopia. Ethiop J Health Dev. 20
- Nathan R, Masanja H, Mshinda H, et al. (2004). Mosquito nets and the poor: can social marketing redress inequities in access? Trop Med Hyg. 9:1121-6
- Muchie KF, Alemu K, Tariku A et al. (2017). Rural households at risk of malaria did not own sufficient insecticide treated nets at Dabat HDSS site: evidence from a cross sectional re-census. BMC Pub heal.17:1-9.
- Tilaye T (2016). Assessment of malaria prevalence and knowledge attitude an d practices (KAP) in relation to malaria prevention and control in Gondar town. North Ethiop Cent Data Cat Addis Ababa Univ.
- Animut A, Negash Y, Kebede N (2014). Distribution and utilization of vector control strategies in a malarious village of Jabi Tehnan District, north-western Ethiopia. Malar J.13:1-6
- US-president’s malaria initiative Ethiopia (. 2019). Ethiopia Malaria Operational Plan.
- Beyene HB, Telele NF, Mekuria AH (2015). Knowledge, attitude and practice on malaria and associated factors among residents in Pawe district, north west Ethiopia: a cross-sectional study. Sci J Pub Healt. 3:303-9
- Abate A, Degarege A, Erko B (2013). Community knowledge, attitude and practice about malaria in a low endemic setting of Shewa Robit Town, northeastern Ethiopia. BMC pub heal.13:1-8
- Aderaw Z, Gedefaw M (2013). Knowledge, attitude and practice of the community towards malaria prevention and control options in anti-malaria association intervention zones of Amahara National Regional State, Ethiopia. J Trop Dis. 1:10-4172
- Aragie TB (2020). Knowledge of malaria prevention and control methods and associated factors among rural households in west Belessa district, north west Ethiopia, 2019. BMC public health. 20:1-7.
- Girum T, Hailemikael G, Wondimu A (2017). Factors affecting prevention and control of malaria among endemic areas of Gurage zone: an implication for malaria elimination in South Ethiopia, 2017. Trop Dis Travel Med 3:1-9
- Luyiga F. Knowledge, attitude and practices on malaria prevention and control in Uganda. Publ Commun Dev Found Uganda CDFU

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences