Aortic Valve Papillary Fibroelastoma Presenting Acute Stroke
Ikuo Fukuda*, Zaiqiang Yu, Kazuyuki Daitoku, Wei Yang
Department of Thoracic and Cardiovascular Surgery, Hirosaki University Graduate School of Medicine, Aomori, Japan
- Corresponding Author:
- Ikuo Fukuda
Department of Thoracic and Cardiovascular Surgery
Hirosaki University Graduate School of Medicine, Aomori, Japan
Tel: +81(172)39-5074
E-mail: ikuofuku@hirosaki-u.ac.jp
Received date: December 03, 2018; Accepted date: December 14, 2018; Published date: December 30, 2018
Citation: Fuduka F, Yu Z, Daitoku K, Yang W. Aortic valve papillary fibroelastoma presenting acute stroke. Electronic J Biol, 14:4
Abstract
Background: Papillary fibroelastoma is uncommon in cardiovascular disease and is found incidentally during surgery or transesophageal echocardiography. Because it presents severe diverse clinical syndromes including acute stroke and chronic angina, timing of operation is an important issue. Case presentation: We report a case of 69-yearold man diagnosed with acute stroke presenting aphasia. Transesophageal echocardiography identified a flail tumor on the non-coronary cusp of aortic valves. Because he had no history of persisting fever, that was regarded as the cause of embolic stroke. The patient underwent simple resection of tumor with aortic valve repair to prevent from recurrence of embolism. Conclusion: Although papillary fibroelastomas does not induces acute stroke frequently, surgical intervention is necessary for preventing from recurrence of embolism. Transesophageal Echocardiography (TEE) is efficacious for differential diagnosis for cardiogenic stroke.
Keywords
Papillary fibroelastomas; Acute stroke; Aortic valve tumor; Case report
Abbreviations
PFEs: Papillary Fibroelastomas; TEE: Transesophageal Echocardiography
Introduction
Papillary Fibroelastom (PFE) is the second most common benign tumor of heart and presents with syndromes including embolic events and chronic angina without coronary artery disease in several patients [1,2]. Transesophageal or Transthoracic Echocardiography (TEE, TTE) is the most effective tool to diagnose PFE preoperative. Surgical excision is necessary if PFE is left-sided flail lesion and greater than 1 cm in diameter. If patient exhibits angina or embolic events, surgical outcome is excellent [3]. We report a case of a 69-year-old man, with acute stroke and incidentally found with PFE on the non-coronary cusp of the aortic leaflets.
Case Presentation
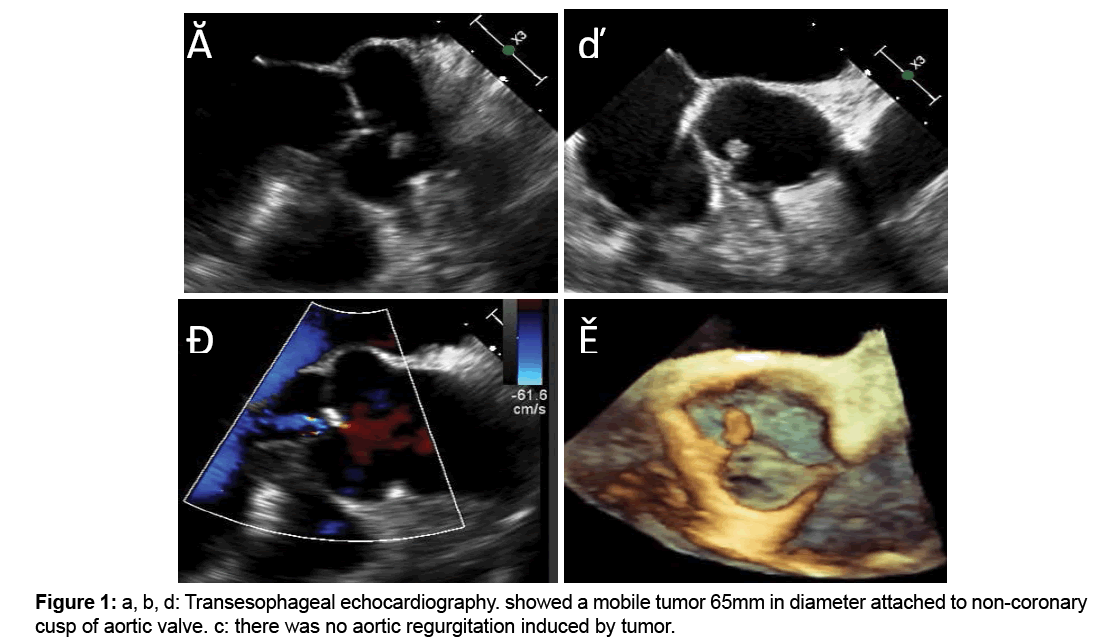
A 69-year-old man who had a history of percutaneous coronary intervention for Acute Myocardial Infarction (AMI) 10 years ago, presenting high blood pressure and dizziness. The patient exhibited aphasia at emergency room which was confirmed and disappeared at next day. Although Computed Tomography (CT) of brain showed no cerebral infarction, Magnetic Resonance Imaging (MRI) demonstrated small old cerebral infarction sections at occipital lobe. Magnetic Resonance Imaging (MRI) showed mild stenosis of right middle cerebral artery which is not relevant to aphasia. Because he had history of Acute Myocardial Infarction (AMI), Transesophageal Echocardiography (TEE) was performed. TEE revealed that a small, rounded and high echoic nudule on the non-coronary cusp. It was flail and sized approximately 10×5 mm (Figure 1). He had no history of persisting or spike fever, so infective endocarditis was excluded. According to its appearances, the diagnosis of Papillary Fibroelastom (PFE) was made. We suspected that PFE was cause the aphasia resulting in debris-embolism or thromboembolism.
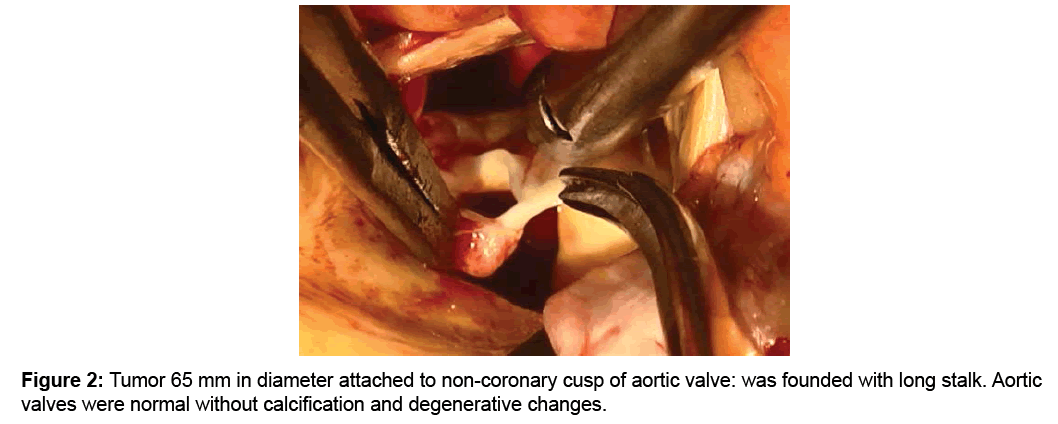
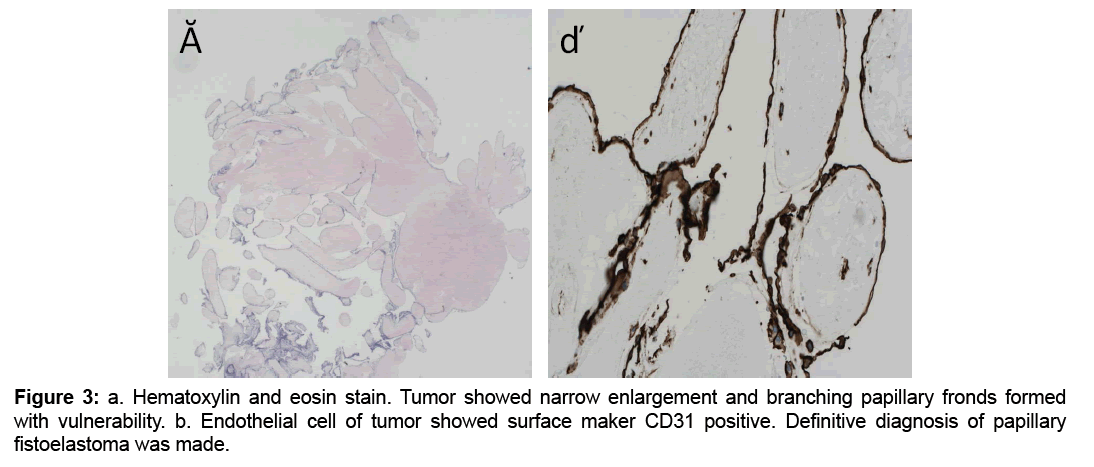
Therefore tumor resection assisted by cardiopulmonary bypass was indicated. Operative findings showed that the tumor adhered to noncoronary cusp by thin stalk (Figure 2), accessary tumor was confirmed on the ventricular side of non-coronary cuspid. We resected tumor without injurying aortic valve cuspid. Postoperative course was uneventful. Definitive pathological diagnosis was PFE (Figure 3). Postoperative TEE showed no aortic regurgitation, there was no tumor recurrence 6 months postoperative.
Discussion
Cardiac PFE is the second most common valvular tumor and histologically benign. It is always found in left-side heart valves, and it sometimes leads to lifethreatening complications including embolic stroke, cardiac arrest or chronic angina [4]. According to universal application of TEE to explore embolic source of cardiovascular origin, it is the most useful for diagnosis of PFEs. However, differential diagnosis of valvular tumor including infective endocarditis, non-bacterial endocarditis and myxoma is difficult [5].
There are several hypotheses about development of PFEs, organizing thrombi, cytomegalovirus infection, rheumatic aortic valve disease or primary neoplasms [6-8]. The presented patient did not have any history of persisting fever, patent foramen ovale, atrial septal aneurysm or aortic atheromatosis, therefore we thought that the reason of cerebral infarction was induced by PFEs. Previous analysis of 21 patients having PFEs showed that 33.3% patients presented cerebral infarction and 9.5% patients showed angina caused by thromboembolism from PFEs [9]. Thromboembolic event is the most important indication for surgery intervention.
What is the best surgical procedure for PFEs? Gowda et al. analysed 725 cases of PFE and 425 patients undergoing surgical treatment, 81% of patients underwent shaving excision, and the rest of patients underwent valve replacement or repair, either procedure did not accompanied no recurrence risk; therefore surgical procedure should be determined according to tumor`s size or local attachment of tumor [2]. Our patient was a 69-year-old man, without aortic valves damaged and regurgitation induced by PFEs, so we performed shaving excision surgery without deterioration valve function. Differentiation of PFEs and myxoma is another important point because myxoma has 5% recurrence without sufficient margins [10]. It is difficult to get definitive diagnosis by macroscope examination during operation. If the tumor shows hairy pattern on inspection, definitive diagnosis is easy without wrong diagnosis risk. And Patients not candidates for surgical treatment should be treated with long-term anticoagulation, but without guidelines [11]. Surgical procedure for PFEs, they are determined mainly according to judgements of cardiology surgeons.
Recently, it has been discovered the contribution of acute and chronic stress in cardiovascular diseases, especially aortic valve calcification, atrial arrhythmia and stroke. Our research group had showed that cytokine tumor necrosis factor-α accelerated aortic valve calcification [12]. Inflammation and oxidative stress increased insulin resistance to cause stroke worse and worse [13]. Stress cardiomyopathy would be induced after a large cerebral infarction [14]. Previous study had acknowledged that the stress kinase c-Jun N-terminal Kinase (JNK) increased incidence of Atrial Fibrillation (AF) by downregulating Cx43 expression [15]. Also alcohol activated JNK to accelerate AF by enhancing cellular CaMKII activity [16]. According to these studies, stress has very deep relationship with cardiovascular disease including PFEs, which need to be further acknowledged in future. This patient had history of paroxysmal atrial fibrillation, and AF occurred postoperative, but which was controlled by oral drugs easily, we suspected that it did not have relationship with cerebral infarction
Conclusion
Although papillary fibroelastomas induces acute stroke not frequently, surgical intervention is necessary for preventing from recurrence of embolism. Long term regularly examinations postoperative need to be performed to follow recurrence and aortic regurgitation.
Authors’ contributions
Study concept and design: ZY and KD, and IF. Acquisition of data: ZY, KD, WY, and IF. Analysis and interpretation of data: ZY, KD, and IF. Drafting of the manuscript: ZY and KD. Critical revision of the manuscript for important intellectual content: All authors. All authors read and approved the final manuscript.
References
- Zhang F, Zhu ZQ, Upadhya GK, et al. (2017). Papillary fibroelastom of the aortic valve presenting with chronic angina and acute stroke: a case report. J Med Case R. 11: 17.
- Gowda RM, Khan IA, Nair CK, et al. (2003). Cardiac papillary fibroelastom: a comprehensive analysis of 725 cases. Am Heart J. 146: 404-10.
- Ngaage DL, Mullany CJ, Daly RC, et al. (2005). Surgical treatment of cardiac papillary fibroelastom: a single center experience with eighty-eight patients. Ann Thorac Surg. 80: 1712-18.
- Yandrapalli S, Mehta B, Mondal P, et al. (2017). Cardiac papillary fibroelastoma: The need for a timely diagnosis. World J Clin Cases. 16: 9-13.
- Kirkpatric JN, Wong T, Bednarz JE, et al. (2004). Differential diagnosis of cardiac masses using contrast echocardiographic perfusion imaging. J Am Coll Cardiol. 43: 1412-1419.
- Molnar A, Encica S, Kovacs E, et al. (2014). Papillary fibroelatoma of the pulmonary valve: A case report. Rom J Morphol Embryol. 55: 463-67.
- Aryal MR, Baral M, Mainali NR, et al. (2013). Papillary fibroelatoma of the aortic valve: An unusual cause of angina. World J Cardiol. 5: 102-105.
- Tamin SS, Maleszewski JJ, Scott CG, et al. (2015). Prognosis and bioepidemiologic implications of papillary fibroelastomas. J Am Coll Cardiol. 65: 2420-2429.
- Ikegami HH, Andrei AC, Li Z, et al. (2015). Papillary fibroelastoma of the aortic valve. Tex Heart Inst J. 42:131-5.
- Parthenakis F, Nyktari E, Patrianakos A, et al. (2009). Asymptomatic papillary fibroelastoma of the aortic valve in a young woman-a case report. Cardiovasc Ultrasound. 7: 43.
- Baikoussis NG, Dedeilias P, Argiriou M, et al. Cardiac papillary fibroelastoma; when, how, why? Ann of Card Anaesth. 19: 162-165.
- Yu Z, Seya K, Daitoku K, et al. (2011). Tumor necrosis factor-α accelerates the calcification of human aortic valve interstitial cells obtained from patients with calcific aortic valve stenosis via the BMP2-Dlx5 pathway. J Pharmacol Exp Ther. 337:16–23.
- Ozkul A, Ayhan M, Akyol A, et al. (2013). The effect of insulin resistance on inflammatory response and oxidative stress in acute cerebral ischemia. Neuro Endocrinol Lett. 2013;34: 52-7.
- Wang Q, Yu H, Jiang C, et al. (2018). Cerebral infarction as initial presentation in stress cardiomyopathy Case report and literature review. Medicine. 97:20.
- Yan J, Thomson J, Zhao W, et al. (2018). The stress kinase JNK regulates gap junction Cx43 gene expression and promotes atrial fibrillation in the aged heart. J Mol Cell Cardiol. 114: 105–115.
- Yan J, Thomson J, Zhao W, et al. (2018). Role of Stress Kinase JNK in Binge Alcohol-Evoked Atrial Arrhythmia. J Am Coll Cardiol. 71: 1459–1470.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences