Current Vaccine Development against Plague
Wei Sun
Wei Sun*
Center for Infectious Disease and Vaccinology,The Biodesign Institute,Arizona State University,Tempe,AZ,85287,USA
Abstract
Yersinia pestis, the causative organism of the plague, has played an important role in shaping human history. Plague is an illness that may manifest in bubonic, pneumonic, or septicemic form. Natural outbreaks devastated entire populations in medieval times and an estimated 200 million humans were killed by plague throughout history. The organism can still be found today throughout the world, including the United States. Approximately 2,000 cases of plague are reported each year to the World Health Organization. The potential use of the bacteria in modern times as an agent of bioterrorism makes understanding this organism a priority. The author reviews the current vaccine development against plague after a brief description of the history of plague pandemics
Keywords
Yersinia pestis; plague; vaccines
1. Introduction
Yersinia pestis,the causative agent of plague,is an aerobic,non-motile,gram-negative bacillus belonging to the family Enterobacteriacea. It is a zoonotic infection transmitted to humans via the bite of a flea. The natural reservoir of Y. pestis is rodents,squirrels,and prairie dogs. It is usually transmitted via the flea Xenopsylla cheopis [1]. Large reservoirs of Y. pestis still exist on all major inhabited continents,except Australia,with a large reservoir being in the southwestern US [2]. In human history,plague are endemic in many parts of the world,including the US,and have resulted in horrible disaster [3]. The first outbreak of plague was documented in 1320 before the common era (BCE) among the Philistines. Biblical reference to this outbreak is found in I Samuel 5:6. In the last two millennia,the plague has reached pandemic proportions affecting many countries on most continents [4]. The first plague pandemic,also referred to as the Justinian Plague,began in Pelusium,Egypt in 541 common era (CE) [2,4,5]. Outbreaks in Europe,Central and Southern Asia,and Africa killed an estimated 100 million people [2,4]. The second pandemic of the fourteenth century (1347 - 1350 CE) began in Sicily and rapidly spread throughout Europe over the next several years,killing an estimated one third of the European population [2,4,5]. During that time,plague became known as "Black Death". Outbreaks of plague continued to occur sporadically in Europe over the next several centuries. The third pandemic began in 1894 in Hong Kong and Canton and in Bombay in 1898. It spread around the world over a ten year period,predominantly from infected rats and their fleas that were aboard steamships [2,4]. An estimated 12 million deaths occurred. Between 1898 and 1908 approximately six million deaths occurred in India alone [6]. Since 1954,an average of ~1,800 confirmed plague cases worldwide per year were recorded by the WHO. The number of yearly cases is highly dependent upon epidemic outbreaks and the reporting of cases to WHO; cases reported to WHO likely represent only a fraction of the total number of cases. The 1994 outbreak of pneumonic plague in India (876 cases with 54 fatalities) highlighted both the potential for serious epidemics and the lack of adequate training of health care personnel in recognizing and dealing with plague [2,7].
2. Materials and Methods
2.1 Study sites and sampling
Three clinical forms of human plague exist: bubonic,pneumonic,and septicemic. Y. pestis cells spread from the site of the infected flea bite to the regional lymph nodes,grow to high numbers causing formation of a bubo,and spill into the blood stream where bacteria are removed in the liver and spleen. Growth continues in the liver and spleen,spreads to other organs,and causes a septicemia. Fleas feeding on septicemic or bacteremic animals complete the life cycle. Humans are accidental hosts that are highly susceptible to plague. In humans bubonic plague can develop into an infection of the lung (secondary pneumonic plague); this can lead to aerosol transmission (primary pneumonic plague) [2,8].
In addition to the potential for natural infections,Y. pestis is generally considered to be among the top five potential biological weapons [9]. One of the earliest recorded biological warfare attempts used plague - Tartar forces,laying siege to 14th-century Kaffar (now called Feodosia,Ukraine),catapulted their plague victims into the city in an attempt to start an epidemic among the defending forces.
During World War II,Japanese forces released plague-infected fleas from aircraft over Chinese cities. More recently,an Ohio man with extremist connections tried to obtain Y. pestis from the American Type Culture Collection and evidence indicates that Y. pestis was being developed for potential biological warfare use in the former Soviet Union. To be effective,a bioterrorism/biowarfare agent must be easily propagated and prepared,easily dispersed with high infectivity,and must cause a rapidly developing,severe disease [9-13]. Plague clearly fulfills these criteria. The organism is readily cultured in a variety of common laboratory growth media. Aerosol dispersal is a proven route of infection that causes pneumonic plague - aerosol delivery of doses as low as ~100 organisms to African green monkeys caused fatal infections [14]. Thus the LD50 of aerosol-delivered plague is likely to be 100-fold lower than that for anthrax spores (LD50 of 5 x 104 in rhesus monkeys) [15]. Pneumonic plague has a short incubation period and progresses rapidly to a highly fatal infection. Victims often become sources of secondary infections as indicated by plague epidemics throughout history [2,8].
Three other factors make Y. pestis an attractive potential biological agent for terrorists or governments. The organism can be easily obtained from any of the numerous and widely dispersed animal reservoirs of plague [2]. Additionally,the emergence of Y. pestis strains resistant to multiple drugs has been isolated from plague patients in Madagascar,which may spread character of multiple antibiotic resistances to plague reservoirs [16,17]. Second,Y. pestis is easily genetically manipulated to create strains with specific engineered traits,such as constructing a super Y. pestis strains resistant to the top 5-6 antibiotics of choice in prompt treatment of plague. Third,currently there is no plague vaccine available for vaccination of the public or military personnel. All those factors make Y. pestis with high potential for use as a bioterrorism/biowarfare agent. Especially in its pneumonic form,Y. pestis has the dubious distinction of being one of the most highly virulent and rapidly fatal causes of acute bacterial infections.
3. Results
Although antibiotics have been used for plague prophylaxis,they are useful only in the setting of a known case of plague. In addition,Although plague infection is associated with high mortality,bubonic plague survivors were considered immune to subsequent infection [18]. The apparent ability to resist infection was the basis for Haffkine’s first plague vaccine [19]. The promise of plague immunity continues to fuel research into the development of safe and efficacious vaccines. The first FDA licensed plague vaccine,USP (Cutter Biological) or Killed Whole-Cell (KWC) vaccine,was a formalin preparation of the fully virulent strain Y. pestis 195/P. The vaccine is considered safe and efficacious at preventing bubonic plague [20,21]. Adverse reactions such as fever,headache,lymphadenopathy and the need for booster injections eventually diminished interest in the USP vaccine. KWC immunization does not generate protective immunity against pneumonic plague [22,23]. As vaccine development has shifted towards preventing pneumonic plague,USP would not be considered efficacious [9]. Therefore,Greer laboratories had stopped manufacturing the only U.S. licensed vaccine [2]. Recent efforts to create a safe and effective plague vaccine have focused on the development of recombinant subunit vaccines that elicit antibodies against two well characterized Y. pestis antigens,the F1 capsule and the virulence protein LcrV [24-27]. But USAMRIID demonstrated that F1/LcrVbased vaccines protect cynomolgus macaques against aerosolized Y. pestis but fail to adequately protect African green monkeys (efficacy ranged from 0% to 75% in five trials) [28].
A number of approaches are underway to improve the efficacy of F1/LcrV-based vaccines [29]. Some researchers are genetically modifying the antigens [30,31],while others are exploring the use of alternate adjuvants [32-35] and delivery platforms using attenuated Salmonella,Y. pseudotuberculosis or virus [36-48]. These approaches are certainly promising. However,as already noted,F1-negative Y. pestis strains exist [14,49-53],and pathogenic Yersinia species express multiple LcrV variants,including some that may not confer cross-protective immunity [54].
Most of the live vaccine strains are derivatives of virulent Y. pestis that contain spontaneously arising mutations within the pigmentation (pgm) locus. Unfortunately,these vaccines can be unstable and sometimes display virulence in non-human primates,even killing experimental animals [20,55-57]. In addition,they frequently cause debilitating fever,malaise,and lymphadenopathy in humans [22]. Safety concerns have limited enthusiasm for the development of live attenuated vaccines in the United States and Europe. However,live attenuated vaccines were administered to tens of millions of humans in Indonesia,Madagascar,and Vietnam,apparently without causing any deaths [58]. Live attenuated vaccines also were studied extensively in the former Soviet Union [22,59,60],and the NIIEG line of pgm-negative strain EV 76 is still in use today in Russia [59,61]. As recently as 2002,USAMRIID researchers noted,‘Despite their drawbacks,there is ample evidence that live attenuated strains of Y. pestis should be considered as potential vaccine candidates’ [57].
Currently,several groups recently described attenuated Y. pestis strains with well-defined genetic modifications that may be useful as live vaccines (Table 1).
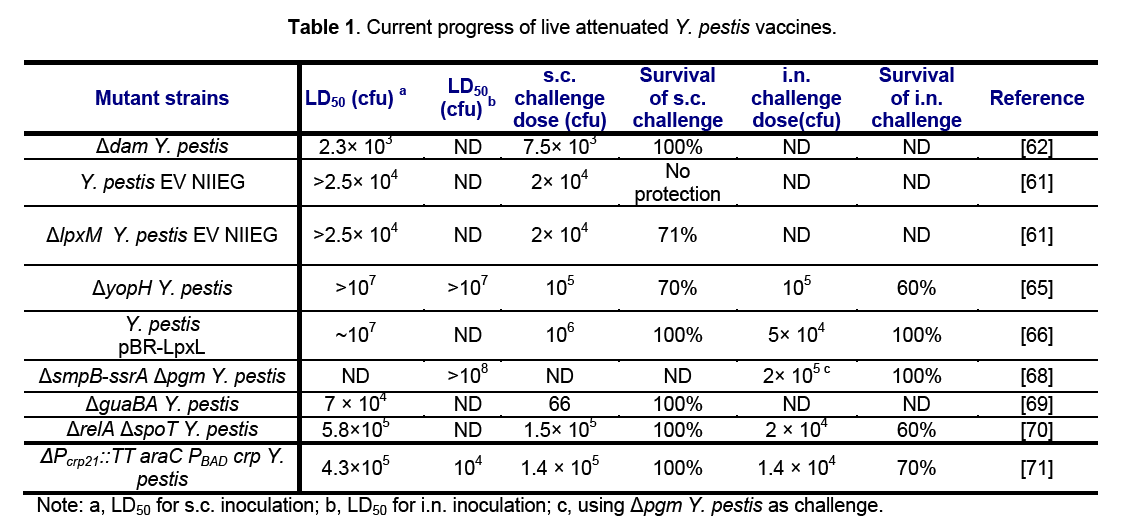
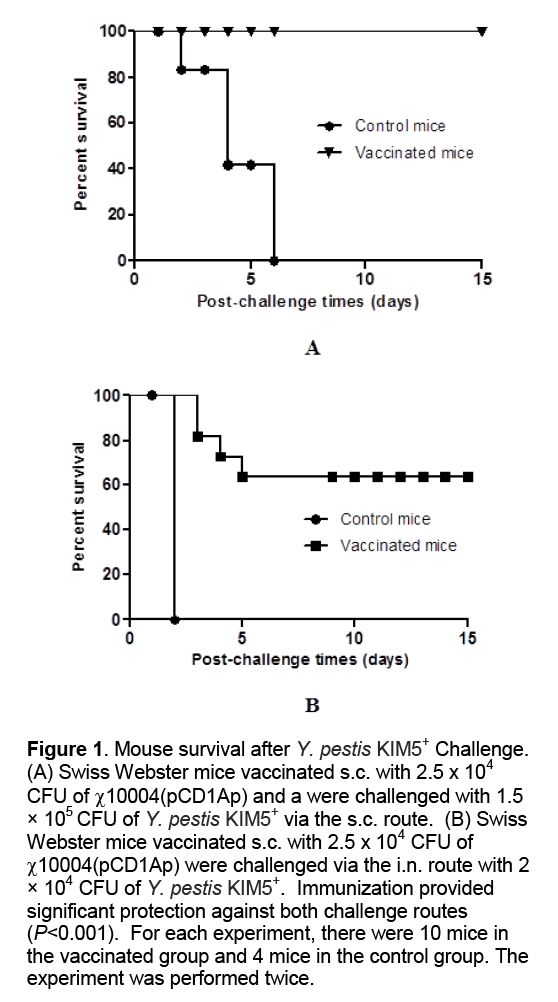
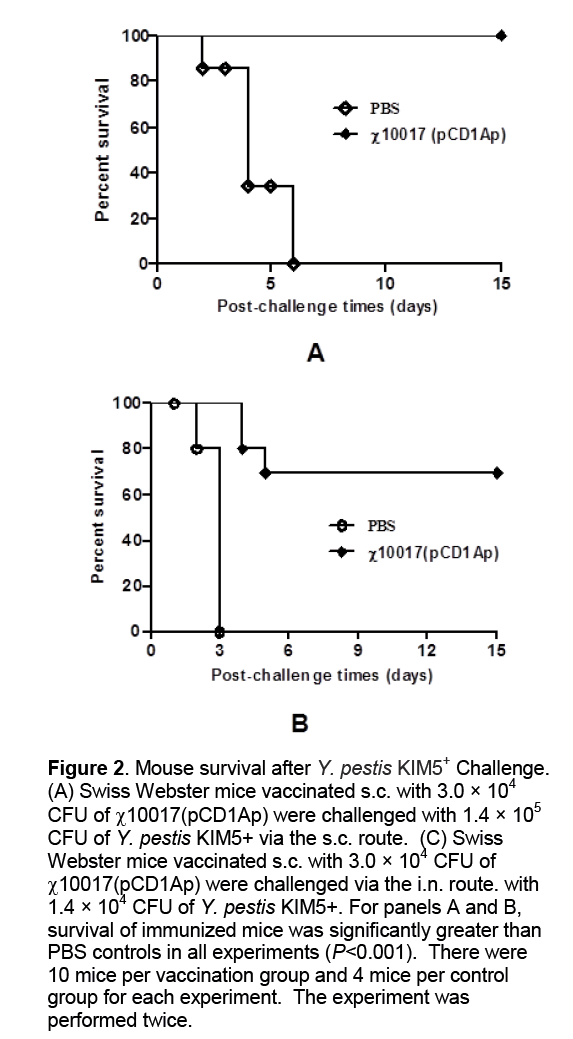
A dam strain of Y. pestis is attenuated and induces protection against plague [62]. The pgm mutant strain primes CD4 and CD8 T cells that synergistically protect against lethal pulmonary Y. pestis infection [63]. A strain with mutations in both the pgm and pla loci safely induces humoral responses in monkeys [57]. Vaccination with strains harboring mutations in both pgm and lpxM loci or only the pgm locus protects mice against subcutaneous challenge [61,64]. Vaccination with a yopH mutant protects mice against both subcutaneous and pulmonary challenge [65]. Vaccination with strains engineered to constitutively produce LPS bearing hexa-acylated lipid A generate very good immungenicity against pneumonic and bubonic plague [66,67]. A smpB- ssrA mutant of Y. pestis functions as a live attenuated vaccine to protect mice against pulmonary plague infection [68] and a guaBA mutant of Y. pestis is attenuated in virulence and provides protection against plague in a mouse model of infection [69]. In our lab,we have constructed relA and spoT double mutant Y. pestis strain and introduced regulated delay system (arabinose regulated Crp expression) into Y. pestis. These two mutants have shown good protective immunogenicity against plague (Figure1 and 2) [70,71].
Figure 1: Mouse survival after Y. pestis KIM5+ Challenge. (A) Swiss Webster mice vaccinated s.c. with 2.5 x 104 CFU of χ10004(pCD1Ap) and a were challenged with 1.5 × 105 CFU of Y. pestis KIM5+ via the s.c. route. (B) Swiss Webster mice vaccinated s.c. with 2.5 x 104 CFU of χ10004(pCD1Ap) were challenged via the i.n. route with 2 × 104 CFU of Y. pestis KIM5+. Immunization provided significant protection against both challenge routes (P<0.001). For each experiment, there were 10 mice in the vaccinated group and 4 mice in the control group. The experiment was performed twice.
Figure 2: Mouse survival after Y. pestis KIM5+ Challenge. (A) Swiss Webster mice vaccinated s.c. with 3.0 × 104 CFU of χ10017(pCD1Ap) were challenged with 1.4 × 105 CFU of Y. pestis KIM5+ via the s.c. route. (C) Swiss Webster mice vaccinated s.c. with 3.0 × 104 CFU of χ10017(pCD1Ap) were challenged via the i.n. route. with 1.4 × 104 CFU of Y. pestis KIM5+. For panels A and B, survival of immunized mice was significantly greater than PBS controls in all experiments (P<0.001). There were 10 mice per vaccination group and 4 mice per control group for each experiment. The experiment was performed twice.
Based on previous investigations,we construct a live attenuated Y. pestis strain that express E. coli lpxL from the chromosome and in combination with the arabinose-regulated crp mutation and show that the double mutant is safer and also provides better protection against bubonic and pneumonic plague than the Pgm-negative mutant. In our investigations,our mutant strain immunization generates complete protection against huge dose of subcutaneous challenge (107 CFU of KIM5+).
We also notice that our mutant strain mutant can give good protection (80% survival) against 100 LD50of KIM5+ by intranasal challenge (intranasal LD50,~100 CFU) (Unpublished data). Our results indicate that this is a very promising finding toward the goal of designing a live safe Y. pestis vaccine that is highly protective against bubonic and pneumonic plague with minimal side effects. Additionally,the potential safety and efficacy of this mutant strain could be enhanced further with additional defined attenuating mutations.
4. Conclusion
Live attenuated versions of virulent pathogens as vectors or vaccines generate broad humoral immune response,but also most effectively prime cellular immunity [72]. Plague vaccines based on live attenuated Y. pestis provide the theoretical advantage of simultaneously priming immunity against many antigens,thereby reducing the likelihood of circumvention by weapon engineers [28]. Therefore,research on the development of new improved live attenuated Y. pestis vaccines should continue and will be strongly encouraged.
References
- Shih C.L SF-Y. (2002) Plague in bioterrorism. Ann Disaster Med,1 Suppl 1.
- Perry R.D,Fetherston J.D. (1997) Yersinia pestis--etiologic agent of plague. Clinical microbiology reviews,10(1): 35-66.
- Human plague in 2000 and 2001. (2003) Wkly Epidemiol Rec,78(16): 130-135.
- Plague. In: WHO report on global surveillance of epidemic-prone infectious diseases. https://wwwwhoint/emc-documents/surveillance/docs/whocdscsrisr2001html/plague/plaguehtm#History Accessed May 28 2003 2000.
- Center for Civilian Biodefense Strategies: Plague fact sheet info http:/ /wwwhopkins-biodefenseorg/pages/agents/agentplaguehtml Accessed May 12 2003.
- Datta K.K. (1994) Plague epidemiology,prevention and control National Institute of Communicable Diseases. Delhi India.
- World H.O. (2003) Human plague in 2000 and 2001. Wkly Epidemiol Rec,78: 130-135.
- Straley S.C.,Starnbach M.N. (2000) Yersinia: strategies that thwart immune defenses. In Cunningham MW (Fujinami R.S.). Effects of Microbes on the Immune System. Philadelphia: Lippincott Williams and Wilkins,
- Inglesby T.V.,Dennis D.T.,Henderson D.A.,Bartlett J.G.,Ascher M.S.,Eitzen E.,et al. (2000) Plague as a biological weapon: medical and public health management. Working Group on Civilian Biodefense. Jama,283(17): 2281-2290.
- Atlas R.M. (1998) The medical threat of biological weapons. Critical reviews in microbiology,24(3): 157-168.
- Danzig R.,Berkowsky P.B. (1997) Why should we be concerned about biological warfare? Jama,278(5): 431-432.
- Henderson D.A. (1998) Bioterrorism as a public health threat. Emerging infectious diseases,4(3): 488-492.
- Inglesby T.V.,Henderson D.A.,O'Toole T.,Dennis D.T. (2000) Safety precautions to limit exposure from plague-infected patients. Jama,284(13): 1648-1649.
- Davis K.J.,Fritz D.L.,Pitt M.L.,Welkos S.L.,Worsham P.L.,Friedlander A.M. (1996) Pathology of experimental pneumonic plague produced by fraction 1-positive and fraction 1-negative Yersinia pestis in African green monkeys (Cercopithecus aethiops). Arch Pathol Lab Med,120(2): 156-163.
- Franz D.R.,Jahrling P.B.,Friedlander A.M.,McClain D.J.,Hoover D.L.,Bryne W.R.,et al. (1997) Clinical recognition and management of patients exposed to biological warfare agents. Jama,278(5): 399-411.
- Guiyoule A.,Rasoamanana B.,Buchrieser C.,Michel P.,Chanteau S.,Carniel E. (1997) Recent emergence of new variants of Yersinia pestis in Madagascar. J Clin Microbiol,35(11): 2826-2833.
- Guiyoule A.,Gerbaud G.,Buchrieser C.,Galimand M.,Rahalison L.,Chanteau S.,et al. (2001) Transferable plasmid-mediated resistance to streptomycin in a clinical isolate of Yersinia pestis. Emerg Infect Dis,7(1): 43-48.
- Simond P-L Y.A. (1900) Peste: bactériologie,symptomatologie,sérothérapie,mesures prophylactiques et thérapeutiques. XIIIe Congrès international de Médecine. Paris: Masson et Cie.
- Haffkine W.M. (1897) Remarks on the plague prophylactic fluid. Br Med J,1: 1461-1462.
- Meyer K.F. (1970) Effectiveness of live or killed plague vaccines in man. Bull World Health Organ,42: 653-666.
- Cavanaugh D.C.,Elisberg B.L.,Llewellyn C.H.,Marshall J.D.,Rust J.H.,Williams J.E.,et al. (1974) Plague immunization. V. Indirect evidence for the efficacy of plague vaccine. J Infect Dis,129(Suppl): S37-40.
- Meyer K.F.,Cavanaugh D.C.,Bartelloni P.J.,Marshall J.D. (1974) Plague immunization. I. Past and present trends. J Infect Dis,129(Suppl): S13-18.
- Titball R.W.,Williamson E.D. (2001) Vaccination against bubonic and pneumonic plague. Vaccine,19(30): 4175-4184.
- Cornelius C.A.,Quenee L.E.,Overheim K.A.,Koster F.,Brasel T.L.,Elli D.,et al. (2008) Immunization with recombinant V10 protects cynomolgus macaques from lethal pneumonic plague. Infect Immun,76(12): 5588-5597.
- Williamson E.D.,Flick-Smith H.C.,Waters E.,Miller J.,Hodgson I.,Le Butt C.S.,et al. (2007) Immunogenicity of the rF1+rV vaccine for plague with identification of potential immune correlates. Microb Pathog,42(1): 11-21.
- Alvarez M.L.,Pinyerd H.L.,Crisantes J.D.,Rigano M.M.,Pinkhasov J.,Walmsley A.M.,et al. (2006) Plant-made subunit vaccine against pneumonic and bubonic plague is orally immunogenic in mice. Vaccine,24(14): 2477-2490.
- Powell B.S.,Andrews G.P.,Enama J.T.,Jendrek S.,Bolt C.,Worsham P.,et al. (2005) Design and testing for a nontagged F1-V fusion protein as vaccine antigen against bubonic and pneumonic plague. Biotechnol Prog,21(5): 1490-1510.
- Smiley S.T. (2008) Immune defense against pneumonic plague. Immunol Rev,225: 256-271.
- Titball R.W.,Williamson E.D. (2004) Yersinia pestis (plague) vaccines. Expert Opin Biol Ther,4(6): 965-73.
- Goodin J.L.,Nellis D.F.,Powell B.S.,Vyas V.V.,Enama J.T.,Wang L.C.,et al. (2007) Purification and protective efficacy of monomeric and modified Yersinia pestis capsular F1-V antigen fusion proteins for vaccination against plague. Protein Expr Purif,53(1): 63-79.
- DeBord K.L.,Anderson D.M.,Marketon M.M.,Overheim K.A.,DePaolo R.W.,Ciletti N.A.,et al. (2006) Immunogenicity and protective immunity against bubonic plague and pneumonic plague by immunization of mice with the recombinant V10 antigen,a variant of LcrV. Infect Immun,74(8): 4910-4914.
- Jones T.,Adamovicz J.J.,Cyr S.L.,Bolt C.R.,Bellerose N.,Pitt L.M.,et al. (2006) Intranasal Protollin/F1-V vaccine elicits respiratory and serum antibody responses and protects mice against lethal aerosolized plague infection. Vaccine,24(10): 1625-1632.
- Glynn A.,Roy C.J.,Powell B.S.,Adamovicz J.J.,Freytag L.C.,Clements J.D. (2005) Protection against aerosolized Yersinia pestis challenge following homologous and heterologous prime-boost with recombinant plague antigens. Infect Immun,73(8): 5256-5261.
- Eyles J.E.,Williamson E.D.,Spiers I.D.,Stagg A.J.,Jones S.M.,Alpar H.O. (2000) Generation of protective immune responses to plague by mucosal administration of microsphere coencapsulated recombinant subunits. J Control Release,63(1-2): 191-200.
- Honko A.N.,Sriranganathan N.,Lees C.J.,Mizel S.B. (2006) Flagellin is an effective adjuvant for immunization against lethal respiratory challenge with Yersinia pestis. Infect Immun,74(2): 1113-1120.
- Oyston P.C.,Williamson E.D.,Leary S.E.,Eley S.M.,Griffin K.F.,Titball R.W. (1995) Immunization with live recombinant Salmonella typhimurium aroA producing F1 antigen protects against plague. Infect Immun,63(2): 563-568.
- Titball R.W.,Howells A.M.,Oyston P.C.,Williamson E.D. (1997) Expression of the Yersinia pestis capsular antigen (F1 antigen) on the surface of an aroA mutant of Salmonella typhimurium induces high levels of protection against plague. Infect Immun,65(5): 1926-1930.
- Leary S.E.,Griffin K.F.,Garmory H.S.,Williamson E.D.,Titball R.W. (1997) Expression of an F1/V fusion protein in attenuated Salmonella typhimurium and protection of mice against plague. Microb Pathog,23(3): 167-179.
- Garmory H.S.,Griffin K.F.,Brown K.A.,Titball R.W. (2003) Oral immunisation with live aroA attenuated Salmonella enterica serovar Typhimurium expressing the Yersinia pestis V antigen protects mice against plague. Vaccine,21(21-22): 3051-3057.
- Yang X.,Hinnebusch B.J.,Trunkle T.,Bosio C.M.,Suo Z.,Tighe M.,et al. (2007) Oral vaccination with salmonella simultaneously expressing Yersinia pestis F1 and V antigens protects against bubonic and pneumonic plague. J Immunol,178(2): 1059-1067.
- Chiuchiolo M.J.,Boyer J.L.,Krause A.,Senina S.,Hackett N.R.,Crystal R.G. (2006) Protective immunity against respiratory tract challenge with Yersinia pestis in mice immunized with an adenovirus-based vaccinevector expressing V antigen. J Infect Dis,194(9): 1249-1257.
- Palin A.,Chattopadhyay A.,Park S.,Delmas G.,Suresh R.,Senina S.,et al. (2007) An optimized vaccine vector based on recombinant vesicular stomatitis virus gives high-level,long-term protection against Yersinia pestis challenge. Vaccine,25(4): 741-750.
- Branger C.G.,Fetherston J.D.,Perry R.D.,Curtiss R.III. (2007) Oral vaccination with different antigens from Yersinia pestis KIM delivered by live attenuated Salmonella typhimurium elicits a protective immune response against plague. Adv Exp Med Biol,603: 387-399.
- Torres-Escobar A.,Juarez-Rodriguez M.D.,Gunn B.M.,Branger C.G.,Tinge S.A.,Curtiss R.,III. (2010) Fine-tuning synthesis of Yersinia pestis LcrV from runaway-like replication balanced-lethal plasmid in a Salmonella enterica serovar typhimurium vaccine induces protection against a lethal Y. pestis challenge in mice. Infect Immun,78(6): 2529-2543.
- Torres-Escobar A.,Juarez-Rodriguez M.D.,Branger C.G.,Curtiss R.III. (2010) Evaluation of the humoral immune response in mice orally vaccinated with live recombinant attenuated Salmonella enterica delivering a secreted form of Yersinia pestis PsaA. Vaccine,28(36): 5810-5816.
- Liu W.T.,Hsu H.L.,Liang C.C.,Chuang C.C.,Lin H.C.,Liu Y.T. (2007) A comparison of immunogenicity and protective immunity against experimental plague by intranasal and/or combined with oral immunization of mice with attenuated Salmonella serovar Typhimurium expressing secreted Yersinia pestis F1 and V antigen. FEMS Immunol Med Microbiol,51(1): 58-69.
- Taylor V.L.,Titball R.W.,Oyston P.C. (2005) Oral immunization with a dam mutant of Yersinia pseudotuberculosis protects against plague. Microbiology,151(Pt 6): 1919-1926.
- Morton M.,Garmory H.S.,Perkins S.D.,O'Dowd A.M.,Griffin K.F.,Turner A.K.,et al. (2004) A Salmonella enterica serovar Typhi vaccine expressing Yersinia pestis F1 antigen on its surface provides protection against plague in mice. Vaccine,22(20):2524-2532.
- Winter C.C.,Cherry W.B.,Moody M.D. (1960) An unusual strain of Pasteurella pestis isolated from a fatal human case of plague. Bull World Health Organ,23: 408-409.
- Friedlander A.M.,Welkos S.L.,Worsham P.L.,Andrews G.P.,Heath D.G.,Anderson G.W.,et al. (1995) Relationship between virulence and immunity as revealed in recent studies of the F1 capsule of Yersinia pestis. Clin Infect Dis,21(Suppl 2): S178-181.
- Welkos S.L.,Davis K.M.,Pitt L.M.,Worsham P.L.,Freidlander A.M. (1995) Studies on the contribution of the F1 capsule-associated plasmid pFra to the virulence of Yersinia pestis. Contrib Microbiol Immunol,13: 299-305.
- Drozdov I.G.,Anisimov A.P.,Samoilova S.V.,Yezhov I.N.,Yeremin S.A.,Karlyshev A.V.,et al. (1995) Virulent non-capsulate Yersinia pestis variants constructed by insertion mutagenesis. J Med Microbiol,42(4): 264-268.
- Worsham P.L.,Stein M.P.,Welkos S.L. (1995) Construction of defined F1 negative mutants of virulent Yersinia pestis. Contrib Microbiol Immunol,13: 325-328.
- Anderson G.W.,Heath D.G.,Bolt C.R.,Welkos S.L.,Friedlander A.M. (1998) Short- and long-term efficacy of single-dose subunit vaccines against Yersinia pestis in mice. Am J Trop Med Hyg,58(6): 793-799.
- Meyer K.F.,Smith G.,Foster L.,Brookman M.,Sung M. (1974) Live,attenuated Yersinia pestis vaccine: virulent in nonhuman primates,harmless to guinea pigs. J Infect Dis,129(Suppl): S 85-120.
- Russell P.,Eley S.M.,Hibbs S.E.,Manchee R.J.,Stagg A.J.,Titball R.W. (1995) A comparison of Plague vaccine,USP and EV76 vaccine induced protection against Yersinia pestis in a murine model. Vaccine,13(16): 1551-1556.
- Welkos S,Pitt ML,Martinez M,Friedlander A,Vogel P,Tammariello R. (2002) Determination of the virulence of the pigmentation-deficient and pigmentation-/plasminogen activator-deficient strains of Yersinia pestis in non-human primate and mouse models of pneumonic plague. Vaccine,20(17-18): 2206-2214.
- Girard G. (1963) Immunity in plague. Acquisitions supplied by 30 years of work ont the "Pasteurella pestis EV" (Girard and Robic) strain. Biol Med (Paris),52: 631-731.
- Zilinskas R.A. (2006) The anti-plague system and the Soviet biological warfare program. Crit Rev Microbiol,32(1): 47-64.
- Aleksandrov N.I.,Gefen N.E.,Gapochko K.G.,Garin N.S.,Daniliuk S.S.,Egorova L.L.,et al. (1963) Study of a Method of Aerosol Immunization with Powdered Plague Vaccine in Extensive Population Groups. Zh Mikrobiol Epidemiol Immunobiol,40: 22-28.
- Feodorova V.A.,Pan'kina L.N.,Savostina E.P.,Sayapina L.V.,Motin V.L.,Dentovskaya S.V.,et al. (2007) A Yersinia pestis lpxM-mutant live vaccine induces enhanced immunity against bubonic plague in mice and guinea pigs. Vaccine,25(44): 7620-7628.
- Robinson V.L.,Oyston P.C.,Titball R.W. (2005) A dam mutant of Yersinia pestis is attenuated and induces protection against plague. FEMS Microbiol Lett,252(2): 251-256.
- Philipovskiy A.V.,Smiley S.T. (2004) Vaccination with live Yersinia pestis primes CD4 and CD8 T cells that synergistically protect against lethal pulmonary Y. pestis infection. Infect Immun,75(2): 878-885.
- Flashner Y.,Mamroud E.,Tidhar A.,Ber R.,Aftalion M.,Gur D.,et al. (2004) Generation of Yersinia pestis attenuated strains by signature-tagged mutagenesis in search of novel vaccine candidates. Infect Immun,72(2): 908-915.
- Bubeck S.S.,Dube P.H. (2007) Yersinia pestis CO92 delta yopH is a potent live,attenuated plague vaccine. Clin Vaccine Immunol,14(9): 1235-1238.
- Montminy S.W.,Khan N.,McGrath S.,Walkowicz M.J.,Sharp F.,Conlon J.E.,et al. (2006) Virulence factors of Yersinia pestis are overcome by a strong lipopolysaccharide response. Nat Immunol,7(10): 1066-1073.
- Szaba F.M.,Kummer L.W.,Wilhelm L.B.,Lin J.S.,Parent M.A.,Montminy-Paquette S.W.,et al. (2009) D27-pLpxL,an avirulent strain of Yersinia pestis,primes T cells that protect against pneumonic plague. Infect Immun,77(10): 4295-4304.
- Okan N.A.,Mena P.,Benach J.L.,Bliska J.B.,Karzai A.W. (2010) The smpB-ssrA mutant of Yersinia pestis functions as a live attenuated vaccine to protect mice against pulmonary plague infection. Infect Immun,78(3): 1284-1293.
- Oyston P.C.,Mellado-Sanchez G.,Pasetti M.F.,Nataro J.P.,Titball R.W.,Atkins H.S. (2010) A Yersinia pestis guaBA mutant is attenuated in virulence and provides protection against plague in a mouse model of infection. Microb Pathog,48(5): 191-195.
- Sun W.,Roland K.L.,Branger C.G.,Kuang X.,Curtiss R.III. (2009) The role of relA and spoT in Yersinia pestis KIM5+ pathogenicity. PLoS One,4(8): e6720.
- Sun W.,Roland K.L.,Kuang X.,Branger C.G.,Curtiss R.III. (2010) Yersinia pestis with regulated delayed attenuation as a vaccine candidate to induce protective immunity against plague. Infect Immun,78(3): 1304-1313.
- Levine M.M.,Sztein M.B. (2004) Vaccine development strategies for improving immunization: the role of modern immunology. Nat Immunol,5(5): 460-464.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences