Abstract
The Comparison of Histopathological Results of the Repair of Dura Defects on Rats Using Different Collagen Based Dura Grafts
Introduction: In cases of celebral cortex damage, such as head traumas or intracranial operations, there is a need to use biocompatible materials (semi-synthetic dural graft) which will allow natural dura formation, prevent the leakage of Cerebral Spinal Fluid (CSF) and which will be completely removed from the body in 3-6 months. Therefore, the spongeous structure of collagen, which is a natural protein of the body, is given membrane form and implanted to the defect area. The aim of this study was to determine the best dura graft by creating a dura mater defect on rats. Methods: A total of 31 female Wistar rats were randomly divided into 5 groups as Group 1 (n=8) dural defect with bovine collagen-origin dura, Group 2 (n=8) dural defect with collagen-based synthetic dura produced from bovine type 1 collagen, Group 3 (n=7) reconstruction with autograft taken from suboccipital fascia, Group 4 (n=5) control group-dural defect with no further procedure and Group 5 (n=3) sham group. At 90 days after the surgical procedures, all the rats were sacrificed under deep anaesthesia. Results: Parenchymal tissue was examined histologically in respect of fibrosis, capillary formation, cellular reaction, capsule formation and foreign body reaction. In leptomeningeal tissues, foreign body reaction, capsule development, integration of artificial brain membrane, inflammation of artificial brain membrane and histological adhesion were examined and the results were compared. While no significant difference was seen between the groups in respect of fibroblastic activity and inflammation, capillary formation was significantly positive in Group 3 autograft and artificial brain membrane integration was significantly positive in Groups 1 and 2, to a greater degree in Group 2, in semi-synthetic collagen based artificial brain membrane. Conclusion: Thus it was concluded that synthetic grafts are adequate and usable in terms of duraplasty.
Author(s):
Mehmet Atif Erol Aksekili, Okan Ateş, Kaan Yüksel, Mahmut Uğurlu, Aydan Kiliçarslan, Nihat Tosun
Abstract | Full-Text | PDF
Share this

Google scholar citation report
Citations : 5001
Electronic Journal of Biology received 5001 citations as per google scholar report
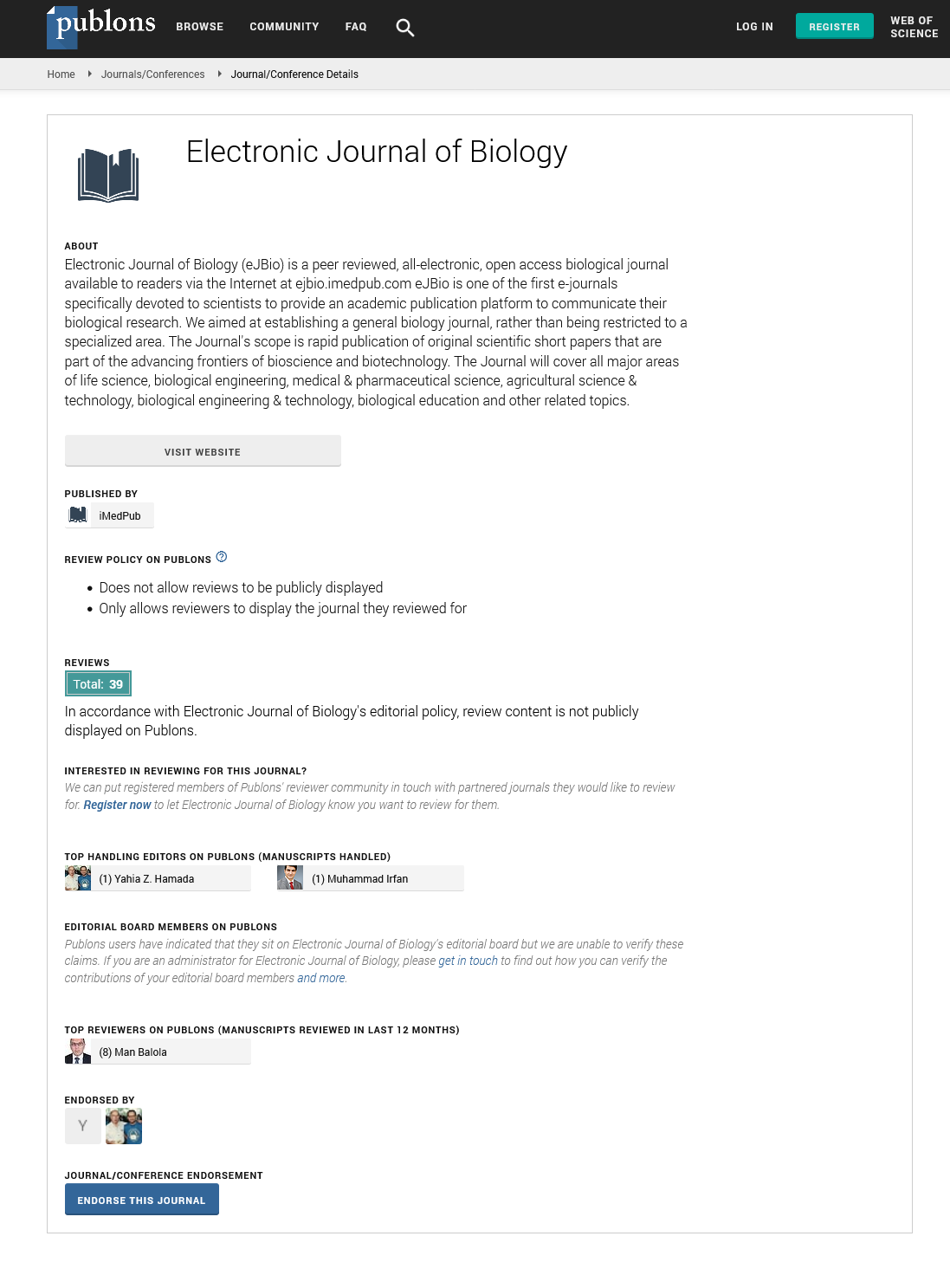
Electronic Journal of Biology peer review process verified at publons
Abstracted/Indexed in
- Google Scholar
- China National Knowledge Infrastructure (CNKI)
- CiteFactor
- Electronic Journals Library
- Zoological Records
- WorldCat
- Proquest Summons
- Publons
- MIAR
- Openaccessarticles.com
- Secret Search Engine Labs
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences